Back

Poster Session A - Sunday Afternoon
Category: Liver
A0563 - A Rare Complication After Transarterial Chemoembolization (TACE): Hepatic Dystrophic Calcification
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Vikash Kumar, MD
The Brooklyn Hospital Center
Brooklyn, NY
Presenting Author(s)
Vikash Kumar, MD, Srilaxmi Gujjula, MD, Praneeth Bandaru, MD, Vijay Gayam, MD, Suut Gokturk, MD, Denzil Etienne, MD, Madhavi Reddy, MD
The Brooklyn Hospital Center, Brooklyn, NY
Introduction: Transarterial chemoembolization (TACE) with radiofrequency ablation (RFA) therapy are considered therapeutic options. It is mostly used in hepatocellular carcinoma (HCC), colorectal, or neuroendocrine tumors. Although it is considered a safe procedure, TACE presents rare complications. We present a case of a 58-year-old female with right sided chest pain who was found to have hepatic calcification seen on chest x-ray after TACE procedure.
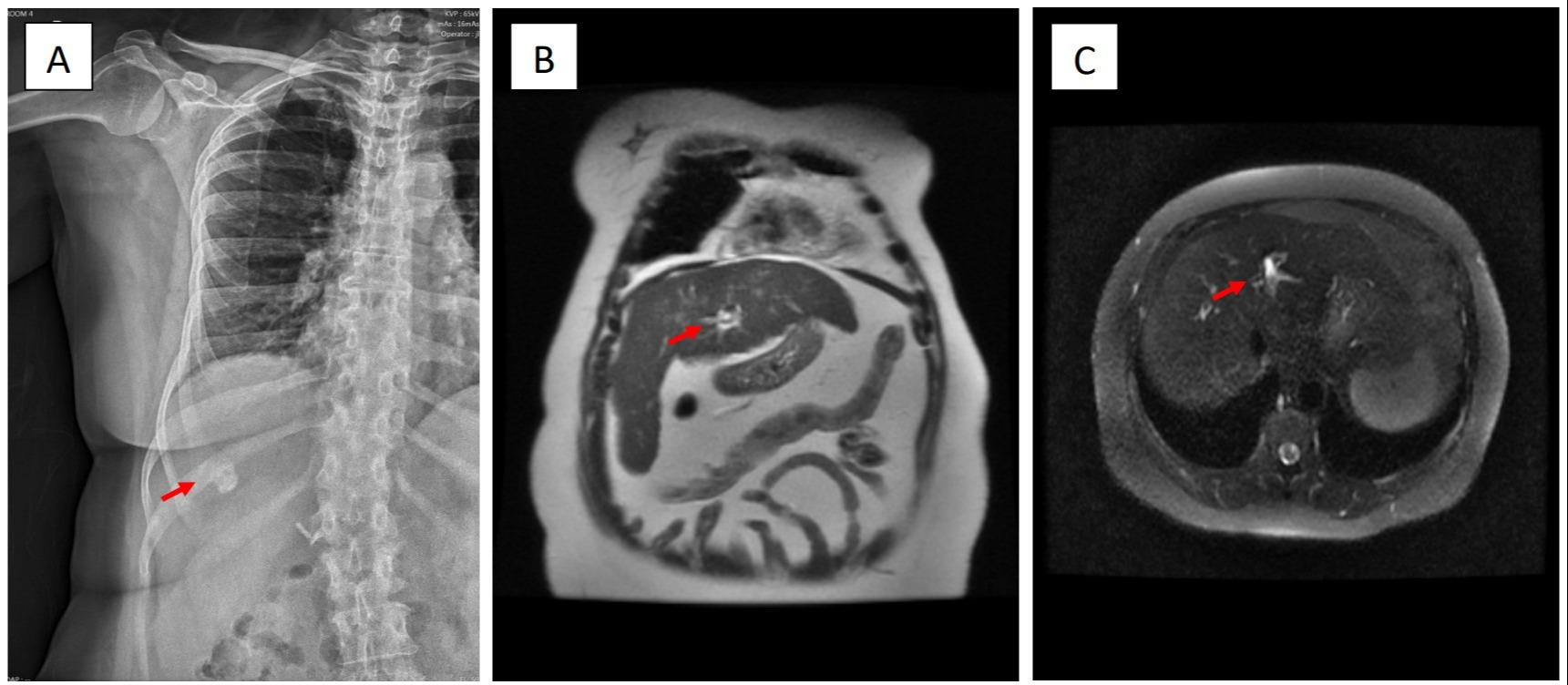
Case Description/Methods: A 58-year-old female with a past medical history of compensated cirrhosis due to hepatitis C virus (HCV) in sustained virologic response (SVR) presented to clinic for follow-up. Alpha-fetoprotein level was elevated to 464. Magnetic resonance imaging (MRI) of abdomen was significant for HCC (Li RADS 5), with no signs of metastatic disease seen on computed tomography (CT) chest and pelvis. The patient was treated with TACE with RFA for early stage of HCC. Six months later, the patient reported chronic intermittent right sided chest and right sided abdominal pain. Physical examination was unremarkable. X-ray chest revealed one-centimeter calcific density projecting over the right upper quadrant of the abdomen (Figure 1A). Repeat MRI of the abdomen showed a stable necrotic treatment cavity and a non-enhancing nodular focus of fat along the posterior aspect of the cavity (Figure 1B, C) without evidence of new HCC. Case was reviewed with a radiologist who deemed the calcification seen on chest x-ray is due to liver directed therapy. Patient was managed conservatively with pain medications.
Discussion: Patients who undergo TACE commonly (about 60%-80% of the time) experience a postembolization syndrome of abdominal pain, fever, and nausea hours to days after the procedure. However, persistent abdominal or chest pain should be evaluated with further imaging. There is a rare possibility of necrosis in the tumor itself even without therapy leading to similar calcification. However, these calcifications are more common after liver directed therapy. Our case demonstrates that a hepatic calcified density can occur as a complication of TACE rather than a de novo tumor in patients with history of HCC and liver directed therapy. This is due to tumor cell necrosis followed by dystrophic calcification which is better seen on x-rays and CT when compared to MRI examination. This case demonstrates a distinctive differential diagnosis of calcified hepatic densities in patients who have previously undergone TACE procedure for HCC.
Disclosures:
Vikash Kumar, MD, Srilaxmi Gujjula, MD, Praneeth Bandaru, MD, Vijay Gayam, MD, Suut Gokturk, MD, Denzil Etienne, MD, Madhavi Reddy, MD. A0563 - A Rare Complication After Transarterial Chemoembolization (TACE): Hepatic Dystrophic Calcification, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
The Brooklyn Hospital Center, Brooklyn, NY
Introduction: Transarterial chemoembolization (TACE) with radiofrequency ablation (RFA) therapy are considered therapeutic options. It is mostly used in hepatocellular carcinoma (HCC), colorectal, or neuroendocrine tumors. Although it is considered a safe procedure, TACE presents rare complications. We present a case of a 58-year-old female with right sided chest pain who was found to have hepatic calcification seen on chest x-ray after TACE procedure.
Case Description/Methods: A 58-year-old female with a past medical history of compensated cirrhosis due to hepatitis C virus (HCV) in sustained virologic response (SVR) presented to clinic for follow-up. Alpha-fetoprotein level was elevated to 464. Magnetic resonance imaging (MRI) of abdomen was significant for HCC (Li RADS 5), with no signs of metastatic disease seen on computed tomography (CT) chest and pelvis. The patient was treated with TACE with RFA for early stage of HCC. Six months later, the patient reported chronic intermittent right sided chest and right sided abdominal pain. Physical examination was unremarkable. X-ray chest revealed one-centimeter calcific density projecting over the right upper quadrant of the abdomen (Figure 1A). Repeat MRI of the abdomen showed a stable necrotic treatment cavity and a non-enhancing nodular focus of fat along the posterior aspect of the cavity (Figure 1B, C) without evidence of new HCC. Case was reviewed with a radiologist who deemed the calcification seen on chest x-ray is due to liver directed therapy. Patient was managed conservatively with pain medications.
Discussion: Patients who undergo TACE commonly (about 60%-80% of the time) experience a postembolization syndrome of abdominal pain, fever, and nausea hours to days after the procedure. However, persistent abdominal or chest pain should be evaluated with further imaging. There is a rare possibility of necrosis in the tumor itself even without therapy leading to similar calcification. However, these calcifications are more common after liver directed therapy. Our case demonstrates that a hepatic calcified density can occur as a complication of TACE rather than a de novo tumor in patients with history of HCC and liver directed therapy. This is due to tumor cell necrosis followed by dystrophic calcification which is better seen on x-rays and CT when compared to MRI examination. This case demonstrates a distinctive differential diagnosis of calcified hepatic densities in patients who have previously undergone TACE procedure for HCC.
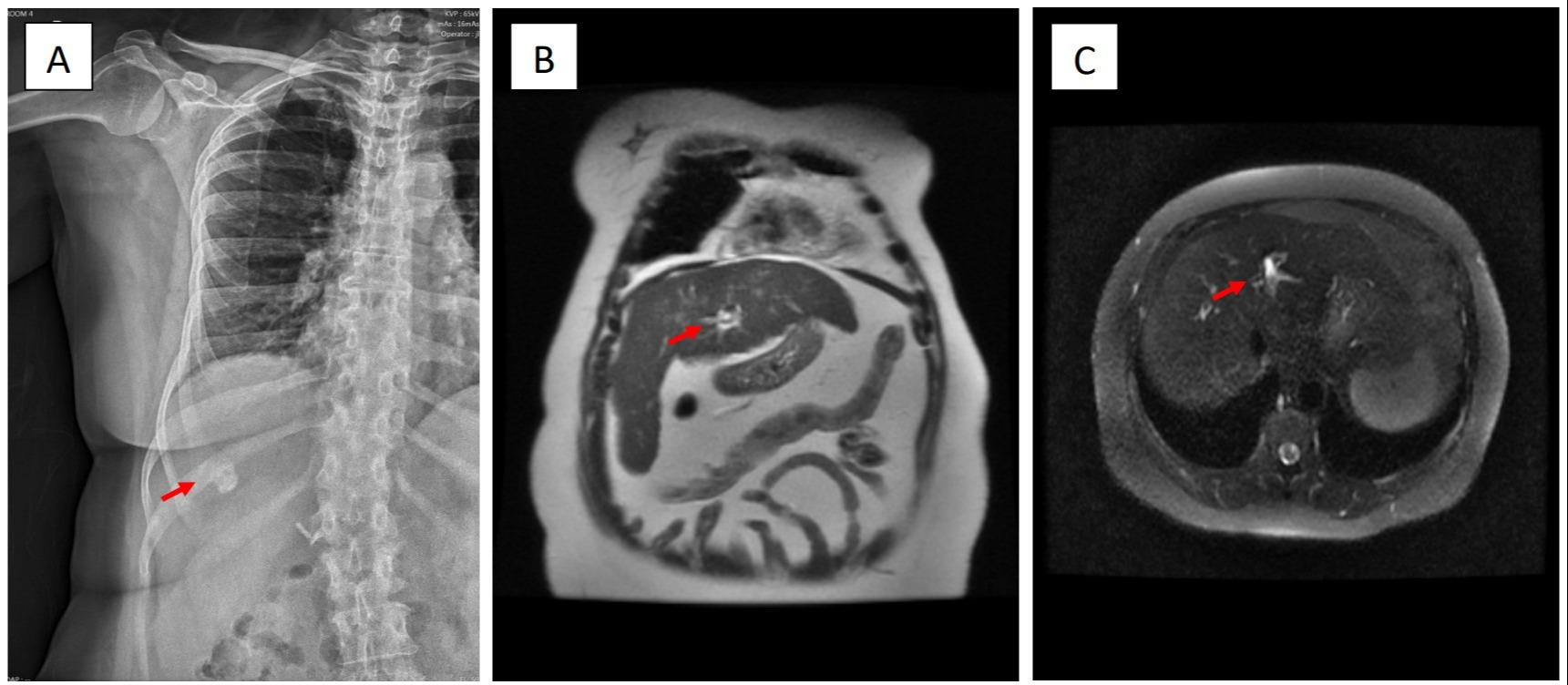
Figure: A: One centimeter calcific density projecting over the right upper quadrant of the abdomen
B, C: Repeat MRI of abdomen showed a stable necrotic treatment cavity and a non-enhancing nodular focus of fat along the posterior aspect of the cavity without evidence of HCC
B, C: Repeat MRI of abdomen showed a stable necrotic treatment cavity and a non-enhancing nodular focus of fat along the posterior aspect of the cavity without evidence of HCC
Disclosures:
Vikash Kumar indicated no relevant financial relationships.
Srilaxmi Gujjula indicated no relevant financial relationships.
Praneeth Bandaru indicated no relevant financial relationships.
Vijay Gayam indicated no relevant financial relationships.
Suut Gokturk indicated no relevant financial relationships.
Denzil Etienne indicated no relevant financial relationships.
Madhavi Reddy indicated no relevant financial relationships.
Vikash Kumar, MD, Srilaxmi Gujjula, MD, Praneeth Bandaru, MD, Vijay Gayam, MD, Suut Gokturk, MD, Denzil Etienne, MD, Madhavi Reddy, MD. A0563 - A Rare Complication After Transarterial Chemoembolization (TACE): Hepatic Dystrophic Calcification, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
