Back

Poster Session B - Monday Morning
Category: Biliary/Pancreas
B0045 - Pneumobilia: A Feature of Ascending Cholangitis Secondary to Periampullary Diverticulum
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Chaitra Banala, MD
Baylor College of Medicine
Houston, TX
Presenting Author(s)
Chaitra Banala, MD, Ankur P. Patel, MD, M. Ellionore Jarbrink-Sehgal, MD, PhD
Baylor College of Medicine, Houston, TX
Introduction: Duodenal diverticula (DD) are found in up to 27% of patients who undergo upper endoscopy, with periampullary duodenal diverticula (PAD) being the most common. While largely asymptomatic, PAD can cause biliary obstruction and related complications. We present a case of ascending cholangitis secondary to extrinsic common bile duct (CBD) compression by a PAD.
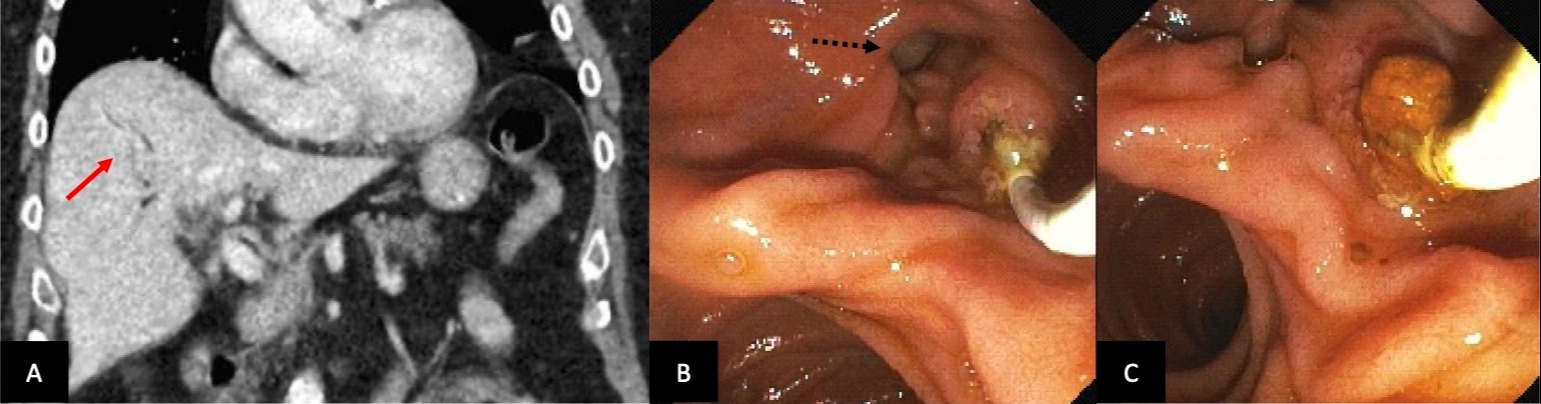
Case Description/Methods: An 82-year-old man with remote cholecystectomy and ulcerative colitis in remission presented with one day of vomiting and abdominal pain. He had no recent endoscopic or surgical interventions. Initial HR was 120 bpm. Vital signs and physical exam were otherwise unremarkable. Labs were notable for WBC 10.7, AST 279, ALT 104, Alk Phos 205 and total bilirubin of 2.9. Abdominal CT revealed pneumobilia of uncertain etiology. Due to concern for ascending cholangitis, antibiotics were initiated. MRCP showed mild central intrahepatic biliary ductal dilation and two CBD filling defects. Blood cultures grew Klebsiella pneumoniae, Escherichia coli, and Streptococcus gallolyticus. In addition to confirming the MRCP findings, ERCP found a large 2 cm PAD. Sphincterotomy and balloon sweeps removed two brown pigmented CBD stones. Occlusion cholangiogram then confirmed successful clearance of filling defects but found a persistent smooth distal CBD narrowing at the area of the PAD, suggestive of extrinsic CBD compression due to the large PAD. Therapeutic decompression with plastic CBD stent placement resulted in immediate clinical and LFT recovery. Final diagnosis was early ascending cholangitis secondary to extrinsic compression by PAD leading to primary choledocholithiasis and bacteremia.
Discussion: While PAD are common, symptomatic presentations are rare and can manifest with CBD dilation, choledocholithiasis, and ascending cholangitis. Lemmel Syndrome is defined by obstructive jaundice caused by a PAD resulting in CBD compression and upstream biliary dilation. We illustrate a case where obstructive jaundice is absent early in the disease course.
Proposed mechanisms include stasis-induced choledocholithiasis secondary to mechanical extrinsic CBD compression and bacterial overgrowth of beta-glucuronidase producing bacteria within the PAD and biliary duct, resulting in deconjugation of bilirubin glucuronides and precipitation of calcium bilirubinate stones. Endoscopic interventions are often successful and sufficient, especially in older patients who may be poor surgical candidates.
Disclosures:
Chaitra Banala, MD, Ankur P. Patel, MD, M. Ellionore Jarbrink-Sehgal, MD, PhD. B0045 - Pneumobilia: A Feature of Ascending Cholangitis Secondary to Periampullary Diverticulum, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Baylor College of Medicine, Houston, TX
Introduction: Duodenal diverticula (DD) are found in up to 27% of patients who undergo upper endoscopy, with periampullary duodenal diverticula (PAD) being the most common. While largely asymptomatic, PAD can cause biliary obstruction and related complications. We present a case of ascending cholangitis secondary to extrinsic common bile duct (CBD) compression by a PAD.
Case Description/Methods: An 82-year-old man with remote cholecystectomy and ulcerative colitis in remission presented with one day of vomiting and abdominal pain. He had no recent endoscopic or surgical interventions. Initial HR was 120 bpm. Vital signs and physical exam were otherwise unremarkable. Labs were notable for WBC 10.7, AST 279, ALT 104, Alk Phos 205 and total bilirubin of 2.9. Abdominal CT revealed pneumobilia of uncertain etiology. Due to concern for ascending cholangitis, antibiotics were initiated. MRCP showed mild central intrahepatic biliary ductal dilation and two CBD filling defects. Blood cultures grew Klebsiella pneumoniae, Escherichia coli, and Streptococcus gallolyticus. In addition to confirming the MRCP findings, ERCP found a large 2 cm PAD. Sphincterotomy and balloon sweeps removed two brown pigmented CBD stones. Occlusion cholangiogram then confirmed successful clearance of filling defects but found a persistent smooth distal CBD narrowing at the area of the PAD, suggestive of extrinsic CBD compression due to the large PAD. Therapeutic decompression with plastic CBD stent placement resulted in immediate clinical and LFT recovery. Final diagnosis was early ascending cholangitis secondary to extrinsic compression by PAD leading to primary choledocholithiasis and bacteremia.
Discussion: While PAD are common, symptomatic presentations are rare and can manifest with CBD dilation, choledocholithiasis, and ascending cholangitis. Lemmel Syndrome is defined by obstructive jaundice caused by a PAD resulting in CBD compression and upstream biliary dilation. We illustrate a case where obstructive jaundice is absent early in the disease course.
Proposed mechanisms include stasis-induced choledocholithiasis secondary to mechanical extrinsic CBD compression and bacterial overgrowth of beta-glucuronidase producing bacteria within the PAD and biliary duct, resulting in deconjugation of bilirubin glucuronides and precipitation of calcium bilirubinate stones. Endoscopic interventions are often successful and sufficient, especially in older patients who may be poor surgical candidates.
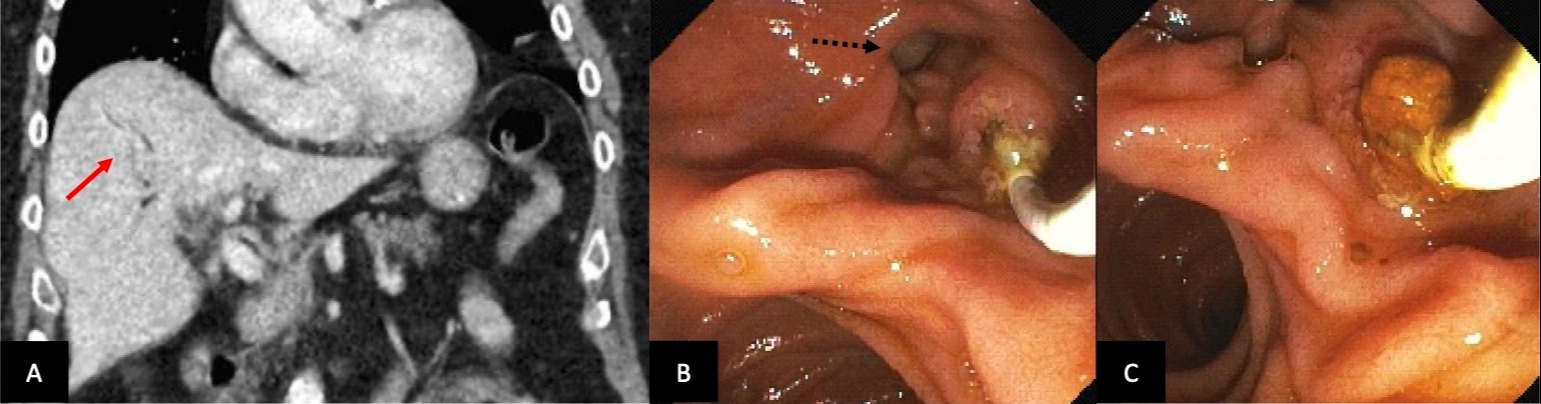
Figure: A. Abdominal CT revealed pneumobila, air within the biliary tree (red arrow). Pneumobilia is most often found after iatrogenic biliary tract manipulation and rarely in emphysematous cholecystitis and biliary-enteric fistulas. However, gas-forming bacteria in cholangitis can also cause pneumobilia, as in our case.
B. ERCP revealed large periampullary duodenal diverticulum (dotted black arrow).
C. Removal of brown pigmented stone from ampulla of Vater.
B. ERCP revealed large periampullary duodenal diverticulum (dotted black arrow).
C. Removal of brown pigmented stone from ampulla of Vater.
Disclosures:
Chaitra Banala indicated no relevant financial relationships.
Ankur Patel indicated no relevant financial relationships.
M. Ellionore Jarbrink-Sehgal indicated no relevant financial relationships.
Chaitra Banala, MD, Ankur P. Patel, MD, M. Ellionore Jarbrink-Sehgal, MD, PhD. B0045 - Pneumobilia: A Feature of Ascending Cholangitis Secondary to Periampullary Diverticulum, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

