Back

Poster Session B - Monday Morning
Category: IBD
B0405 - Predictors and Outcomes of 90-Day Readmission in Inflammatory Bowel Disease Patients Admitted for Percutaneous Coronary Intervention
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- MA
Mohamed K. Ahmed, MD
University of Missouri Kansas City School of Medicine
Kansas City, MO
Presenting Author(s)
Mohamed K. Ahmed, MD1, Wael T. Mohamed, MD2, Abdelrhman Abumoawad, MD3, Ahmed Elkafrawy, MD4, Christina Gomez, MD1, Hassan Ghoz, MD1, Wendell Clarkston, MD5
1University of Missouri Kansas City School of Medicine, Kansas City, MO; 2University of Missouri, Kansas City, MO; 3University of Missouri-Kansas City, Kansas City, KS; 4University of Iowa Hospitals and Clinics, Iowa City, IA; 5University of Missouri-Kansas City School of Medicine, Saint Luke's Hospital, Kansas City, MO
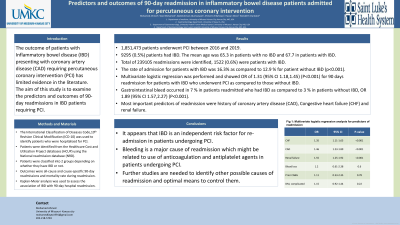
Introduction: The outcome of patients with Inflammatory bowel disease (IBD) presenting with coronary artery disease (CAD) requiring percutaneous coronary intervention (PCI) has limited evidence in the literature. The aim of this study is to examine the predictors and outcomes of 90-day readmissions in IBD patients requiring PCI.
Methods: The International Classification of Diseases Code,10th Revision Clinical Modification (ICD-10) was used to identify patients who were hospitalized for PCI. Patients were identified from the Healthcare Cost and Utilization Project databases (HCUP) using the National readmission database (NRD) between 2016 and 2019. Patients were classified into 2 groups depending on whether they have IBD or not. Outcomes were all-cause and cause-specific 90-day readmissions and mortality rate during readmission. Multiple logistic regression model was used to identify the factors associated with readmission
Results: 1,851,473 patients underwent PCI between 2016 and 2019. 9295 (0.5%) patients had IBD. The mean age was 65.3 in patients with no IBD and 67.7 in patients with IBD. Total of 239105 readmissions were identified, 1522 (0.6%) were patients with IBD. The rate of admission for patients with IBD was 16.3% as compared to 12.9 % for patient without IBD (p< 0.001). Multivariate logistic regression was performed and showed OR of 1.31 (95% CI 1.18,1.455) (P< 0.001) for 90 days readmission for patients with IBD who underwent PCI as compared to those without IBD. Gastrointestinal bleed occurred in 7 % in patients readmitted who had IBD as compared to 3 % in patients without IBD, OR 1.89 (95% CI 1.57,2.27) (P< 0.001). Most important predictors of readmission were history of coronary artery disease (CAD), Congestive heart failure (CHF) and renal failure.
Discussion: It appears that IBD is an independent risk factor for re-admission in patients undergoing PCI. Bleeding is a major cause of readmission which might be related to use of anticoagulation and antiplatelet agents in patients undergoing PCI. Further studies are needed to identify other possible causes of readmission and optimal means to control them.
Disclosures:
Mohamed K. Ahmed, MD1, Wael T. Mohamed, MD2, Abdelrhman Abumoawad, MD3, Ahmed Elkafrawy, MD4, Christina Gomez, MD1, Hassan Ghoz, MD1, Wendell Clarkston, MD5. B0405 - Predictors and Outcomes of 90-Day Readmission in Inflammatory Bowel Disease Patients Admitted for Percutaneous Coronary Intervention, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Missouri Kansas City School of Medicine, Kansas City, MO; 2University of Missouri, Kansas City, MO; 3University of Missouri-Kansas City, Kansas City, KS; 4University of Iowa Hospitals and Clinics, Iowa City, IA; 5University of Missouri-Kansas City School of Medicine, Saint Luke's Hospital, Kansas City, MO
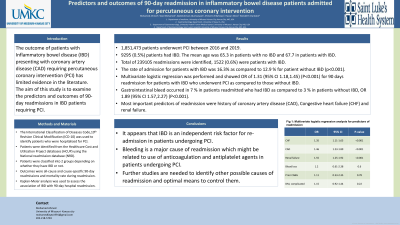
Introduction: The outcome of patients with Inflammatory bowel disease (IBD) presenting with coronary artery disease (CAD) requiring percutaneous coronary intervention (PCI) has limited evidence in the literature. The aim of this study is to examine the predictors and outcomes of 90-day readmissions in IBD patients requiring PCI.
Methods: The International Classification of Diseases Code,10th Revision Clinical Modification (ICD-10) was used to identify patients who were hospitalized for PCI. Patients were identified from the Healthcare Cost and Utilization Project databases (HCUP) using the National readmission database (NRD) between 2016 and 2019. Patients were classified into 2 groups depending on whether they have IBD or not. Outcomes were all-cause and cause-specific 90-day readmissions and mortality rate during readmission. Multiple logistic regression model was used to identify the factors associated with readmission
Results: 1,851,473 patients underwent PCI between 2016 and 2019. 9295 (0.5%) patients had IBD. The mean age was 65.3 in patients with no IBD and 67.7 in patients with IBD. Total of 239105 readmissions were identified, 1522 (0.6%) were patients with IBD. The rate of admission for patients with IBD was 16.3% as compared to 12.9 % for patient without IBD (p< 0.001). Multivariate logistic regression was performed and showed OR of 1.31 (95% CI 1.18,1.455) (P< 0.001) for 90 days readmission for patients with IBD who underwent PCI as compared to those without IBD. Gastrointestinal bleed occurred in 7 % in patients readmitted who had IBD as compared to 3 % in patients without IBD, OR 1.89 (95% CI 1.57,2.27) (P< 0.001). Most important predictors of readmission were history of coronary artery disease (CAD), Congestive heart failure (CHF) and renal failure.
Discussion: It appears that IBD is an independent risk factor for re-admission in patients undergoing PCI. Bleeding is a major cause of readmission which might be related to use of anticoagulation and antiplatelet agents in patients undergoing PCI. Further studies are needed to identify other possible causes of readmission and optimal means to control them.
Disclosures:
Mohamed Ahmed indicated no relevant financial relationships.
Wael Mohamed indicated no relevant financial relationships.
Abdelrhman Abumoawad indicated no relevant financial relationships.
Ahmed Elkafrawy indicated no relevant financial relationships.
Christina Gomez indicated no relevant financial relationships.
Hassan Ghoz indicated no relevant financial relationships.
Wendell Clarkston indicated no relevant financial relationships.
Mohamed K. Ahmed, MD1, Wael T. Mohamed, MD2, Abdelrhman Abumoawad, MD3, Ahmed Elkafrawy, MD4, Christina Gomez, MD1, Hassan Ghoz, MD1, Wendell Clarkston, MD5. B0405 - Predictors and Outcomes of 90-Day Readmission in Inflammatory Bowel Disease Patients Admitted for Percutaneous Coronary Intervention, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
