Back

Poster Session C - Monday Afternoon
Category: Biliary/Pancreas
C0018 - More Than Just an Itch: Impact of Cholestatic Pruritus in Primary Biliary Cholangitis (PBC) on Health-Related Quality of Life (HRQoL)
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Megan M. McLaughlin
GSK
Collegeville, PA
Presenting Author(s)
Helen Smith1, James Fettiplace, MD2, Robyn Von Maltzahn, 2, Sugato Das, 3, Megan M. McLaughlin4, David Jones, 5
1GlaxoSmithKline, London, England, United Kingdom; 2GSK, London, England, United Kingdom; 3GlaxoSmithKline, Hyderabad, Telangana, India; 4GSK, Collegeville, PA; 5Newcastle University, Newcastle, England, United Kingdom
Introduction: Pruritus associated with PBC affects sleep and social and emotional wellbeing. Limited data exist on the impact of pruritus on health utility (a value between 0 [death] and 1 [perfect health]), commonly used in health technology assessments to calculate quality-adjusted life years and compare different conditions. A recent UK study explored EQ-5D utilities in a broad PBC population.1 Here, using data from the Phase 2b GLIMMER study (post hoc) investigating linerixibat for the treatment of pruritus in PBC (NCT02966834), the impact of itch severity on health utility in PBC is explored and quantified for the first time.
Methods: Patients in GLIMMER recorded itch twice daily on a 0–10 numeric rating scale (NRS) and completed the EQ-5D-5L at study entry, baseline (BL) and end of treatment. BL followed a 4-week single-blind placebo run-in. Patients were classed as having mild (< 4), moderate (≥4 to < 7) or severe pruritus (≥7 to 10) based on mean Worst Daily Itch NRS score in the 7 days prior to BL.
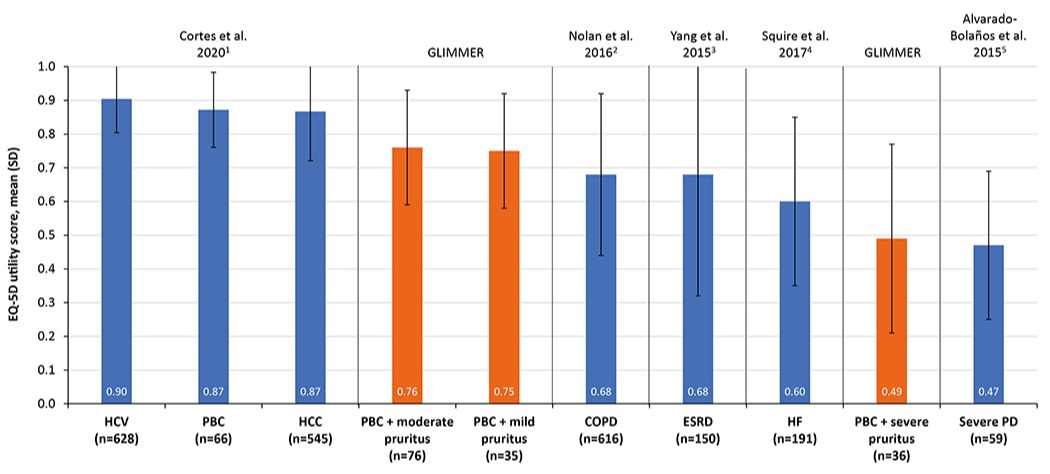
Results: The GLIMMER population (N=147) was 94% female with a mean (SD) age at BL of 55.8 (11.04) years. Most patients had moderate pruritus (n=76), with similar numbers with mild (n=35) and severe (n=36) pruritus. At BL, alkaline phosphatase levels were higher with greater itch severity: mean (SD) 177 (115.4) and 249 (190.8) IU/L in patients with mild and severe itch, respectively. Overall, mean (SD) BL utility was 0.69 (0.23), lower than the general PBC population (Figure) and with a clear and notable impact of pruritus severity on health utility. Thus, patients with mild or moderate pruritus at BL had similar utilities (0.75 [0.17] and 0.76 [0.17], respectively), marginally lower than the general UK population (mean at age 55–64 years: 0.804). Patients with severe pruritus at BL had notably worse utility (0.49 [0.28]), similar to patients with severe Parkinson’s disease (0.47 [0.22]; Figure). Over the course of the study health utility declined in the placebo group (–0.01) and increased across all linerixibat arms (0.04–0.05). Although improvements were small (confidence intervals crossed zero), the directional change supports a treatment effect of linerixibat.
Discussion: Pruritus (particularly severe pruritus) has a significant negative impact on HRQoL and health utility. Presence and severity of itch should be evaluated in PBC and prioritized in treatment plans.
1. Rice et al. Clin Gastroenterol Hepatol 2021;19:769–76.
Disclosures:
Helen Smith1, James Fettiplace, MD2, Robyn Von Maltzahn, 2, Sugato Das, 3, Megan M. McLaughlin4, David Jones, 5. C0018 - More Than Just an Itch: Impact of Cholestatic Pruritus in Primary Biliary Cholangitis (PBC) on Health-Related Quality of Life (HRQoL), ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1GlaxoSmithKline, London, England, United Kingdom; 2GSK, London, England, United Kingdom; 3GlaxoSmithKline, Hyderabad, Telangana, India; 4GSK, Collegeville, PA; 5Newcastle University, Newcastle, England, United Kingdom
Introduction: Pruritus associated with PBC affects sleep and social and emotional wellbeing. Limited data exist on the impact of pruritus on health utility (a value between 0 [death] and 1 [perfect health]), commonly used in health technology assessments to calculate quality-adjusted life years and compare different conditions. A recent UK study explored EQ-5D utilities in a broad PBC population.1 Here, using data from the Phase 2b GLIMMER study (post hoc) investigating linerixibat for the treatment of pruritus in PBC (NCT02966834), the impact of itch severity on health utility in PBC is explored and quantified for the first time.
Methods: Patients in GLIMMER recorded itch twice daily on a 0–10 numeric rating scale (NRS) and completed the EQ-5D-5L at study entry, baseline (BL) and end of treatment. BL followed a 4-week single-blind placebo run-in. Patients were classed as having mild (< 4), moderate (≥4 to < 7) or severe pruritus (≥7 to 10) based on mean Worst Daily Itch NRS score in the 7 days prior to BL.
Results: The GLIMMER population (N=147) was 94% female with a mean (SD) age at BL of 55.8 (11.04) years. Most patients had moderate pruritus (n=76), with similar numbers with mild (n=35) and severe (n=36) pruritus. At BL, alkaline phosphatase levels were higher with greater itch severity: mean (SD) 177 (115.4) and 249 (190.8) IU/L in patients with mild and severe itch, respectively. Overall, mean (SD) BL utility was 0.69 (0.23), lower than the general PBC population (Figure) and with a clear and notable impact of pruritus severity on health utility. Thus, patients with mild or moderate pruritus at BL had similar utilities (0.75 [0.17] and 0.76 [0.17], respectively), marginally lower than the general UK population (mean at age 55–64 years: 0.804). Patients with severe pruritus at BL had notably worse utility (0.49 [0.28]), similar to patients with severe Parkinson’s disease (0.47 [0.22]; Figure). Over the course of the study health utility declined in the placebo group (–0.01) and increased across all linerixibat arms (0.04–0.05). Although improvements were small (confidence intervals crossed zero), the directional change supports a treatment effect of linerixibat.
Discussion: Pruritus (particularly severe pruritus) has a significant negative impact on HRQoL and health utility. Presence and severity of itch should be evaluated in PBC and prioritized in treatment plans.
1. Rice et al. Clin Gastroenterol Hepatol 2021;19:769–76.
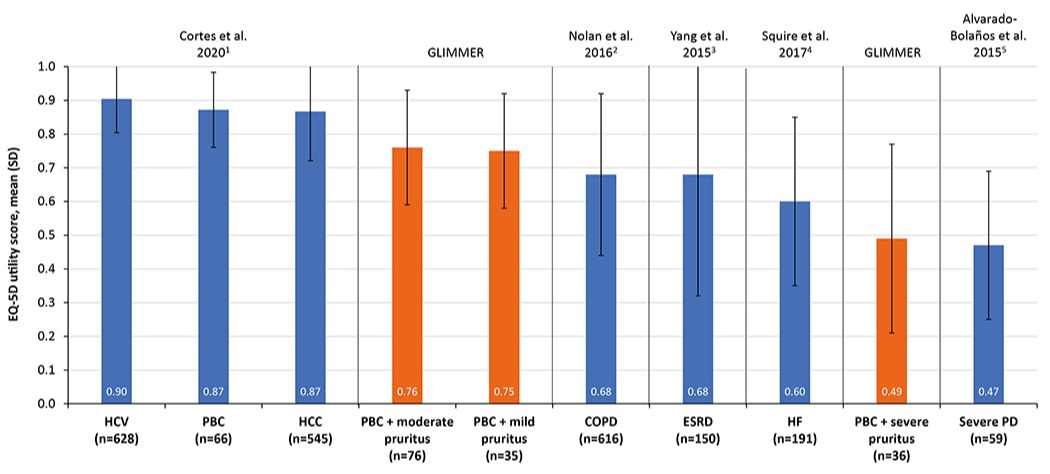
Figure: Figure: Baseline utility scores in PBS patients with cholestatic pruritis (GLIMMER) compared with those seen in other chronic conditions.
1. Cortesi PA, et al. Liver International 2020;40:2630–42; 2. Nolan CM, et al. Thorax 2016;71:493–500; 3. Yang, F et al. Eur J Health Econ 2015;16:1019–26; 4. Squire I, et al. Br J Cardiol 2017;24:30–4; 5. Alvarado-Bolaños A, et al., J Neurol Sci 2015;358:53–7.
COPD, chronic obstructive pulmonary disease; ESRD, end-stage renal disease; HCC, hepatocellular carcinoma; HCV, hepatitis C; HF, heart failure; PBC, primary biliary cholangitis; PD, Parkinson’s disease.
1. Cortesi PA, et al. Liver International 2020;40:2630–42; 2. Nolan CM, et al. Thorax 2016;71:493–500; 3. Yang, F et al. Eur J Health Econ 2015;16:1019–26; 4. Squire I, et al. Br J Cardiol 2017;24:30–4; 5. Alvarado-Bolaños A, et al., J Neurol Sci 2015;358:53–7.
COPD, chronic obstructive pulmonary disease; ESRD, end-stage renal disease; HCC, hepatocellular carcinoma; HCV, hepatitis C; HF, heart failure; PBC, primary biliary cholangitis; PD, Parkinson’s disease.
Disclosures:
Helen Smith: GlaxoSmithKline – Employee, Stock Options.
James Fettiplace: GlaxoSmithKline – Employee, Stock Options.
Robyn Von Maltzahn: GlaxoSmithKline – Employee, Stock Options.
Sugato Das: GlaxoSmithKline – Employee.
Megan McLaughlin: GlaxoSmithKline – Employee, Stock Options.
David Jones: Abbott – Grant/Research Support. Falk – Grant/Research Support. GlaxoSmithKline – Grant/Research Support. Intercept Pharmaceuticals – Grant/Research Support. Novartis – Grant/Research Support. Pfizer – Grant/Research Support.
Helen Smith1, James Fettiplace, MD2, Robyn Von Maltzahn, 2, Sugato Das, 3, Megan M. McLaughlin4, David Jones, 5. C0018 - More Than Just an Itch: Impact of Cholestatic Pruritus in Primary Biliary Cholangitis (PBC) on Health-Related Quality of Life (HRQoL), ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
