Back

Poster Session C - Monday Afternoon
Category: Biliary/Pancreas
C0048 - The Path of Least Resistance: A Case of the Lemmel
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Hardeep S. Ahdi, DO
Advocate Lutheran General Hospital
Chicago, IL
Presenting Author(s)
Hardeep S. Ahdi, DO1, Assad Munis, DO2, Asif Lakha, MD2
1Advocate Lutheran General Hospital, Chicago, IL; 2Advocate Lutheran General Hospital, Park Ridge, IL
Introduction: Lemmel Syndrome is defined as obstructive jaundice caused by a periampullary duodenal diverticulum (PAD) compressing the intrapancreatic common bile duct (CBD) with resultant bile duct dilatation and obstruction. Management is based on symptomatology, ranging from conservative management to endoscopic extraction of retained food debris, or surgery. We present a unique case of Lemmel Syndrome in a patient who suffered from recurrent obstructive jaundice and underwent multiple endoscopic and ultimately, surgical interventions
Case Description/Methods: A 56-year-old obese female with a history of alcohol use disorder initially presented with right upper quadrant abdominal pain for 2 days. Physical exam was remarkable for right upper quadrant tenderness. Labs revealed total bilirubin 3 mg/dL. Complete blood count was within normal limits. Viral hepatitis panel and CA 19-9 were unremarkable. Ultrasound gallbladder showed cholelithiasis without cholecystitis with mild CBD dilatation. MRCP revealed a large 6 cm multiloculated mass centered near the pancreatic head/ampulla of Vater, with internal heterogeneity and multiple air-fluid levels and internally contiguous with duodenal lumen. She was given broad spectrum antibiotics and an upper endoscopy with endoscopic ultrasound was performed revealing a large, non-bleeding periampullary diverticulum impacted with food debris. The food debris was extracted. Multiple such procedures were needed in a short period of time. She continued to suffer from recurrent obstructive jaundice for several months, requiring a cholecystectomy, Roux-En Y hepaticojejunostomy, and gastric antrum resection with Roux-En Y BillRoth II gastrojejunostomy in an attempt to divert food debris away from the diverticulum. She has now developed stenosis at the hepaticojejunostomy requiring ERCP with dilation of the anastomosis, and stenting, as well as percutaneous transhepatic cholangiography, internal external biliary drain placement, lithotripsy of hepatic duct stones, and covered metal stent placement
Discussion: Treatment of Lemmel Syndrome incorporates a variety of modalities. A conservative approach is usually preferred, but invasive intervention may sometimes be required. The most definitive approach would be a Whipple procedure. However, in an obese patient, this would be associated with significant morbidity and mortality risk. Our case portrays an unusual approach which offered the patient a less invasive combined endoscopic, interventional radiology and surgical treatment

Disclosures:
Hardeep S. Ahdi, DO1, Assad Munis, DO2, Asif Lakha, MD2. C0048 - The Path of Least Resistance: A Case of the Lemmel, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Advocate Lutheran General Hospital, Chicago, IL; 2Advocate Lutheran General Hospital, Park Ridge, IL
Introduction: Lemmel Syndrome is defined as obstructive jaundice caused by a periampullary duodenal diverticulum (PAD) compressing the intrapancreatic common bile duct (CBD) with resultant bile duct dilatation and obstruction. Management is based on symptomatology, ranging from conservative management to endoscopic extraction of retained food debris, or surgery. We present a unique case of Lemmel Syndrome in a patient who suffered from recurrent obstructive jaundice and underwent multiple endoscopic and ultimately, surgical interventions
Case Description/Methods: A 56-year-old obese female with a history of alcohol use disorder initially presented with right upper quadrant abdominal pain for 2 days. Physical exam was remarkable for right upper quadrant tenderness. Labs revealed total bilirubin 3 mg/dL. Complete blood count was within normal limits. Viral hepatitis panel and CA 19-9 were unremarkable. Ultrasound gallbladder showed cholelithiasis without cholecystitis with mild CBD dilatation. MRCP revealed a large 6 cm multiloculated mass centered near the pancreatic head/ampulla of Vater, with internal heterogeneity and multiple air-fluid levels and internally contiguous with duodenal lumen. She was given broad spectrum antibiotics and an upper endoscopy with endoscopic ultrasound was performed revealing a large, non-bleeding periampullary diverticulum impacted with food debris. The food debris was extracted. Multiple such procedures were needed in a short period of time. She continued to suffer from recurrent obstructive jaundice for several months, requiring a cholecystectomy, Roux-En Y hepaticojejunostomy, and gastric antrum resection with Roux-En Y BillRoth II gastrojejunostomy in an attempt to divert food debris away from the diverticulum. She has now developed stenosis at the hepaticojejunostomy requiring ERCP with dilation of the anastomosis, and stenting, as well as percutaneous transhepatic cholangiography, internal external biliary drain placement, lithotripsy of hepatic duct stones, and covered metal stent placement
Discussion: Treatment of Lemmel Syndrome incorporates a variety of modalities. A conservative approach is usually preferred, but invasive intervention may sometimes be required. The most definitive approach would be a Whipple procedure. However, in an obese patient, this would be associated with significant morbidity and mortality risk. Our case portrays an unusual approach which offered the patient a less invasive combined endoscopic, interventional radiology and surgical treatment

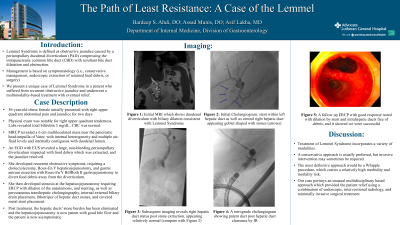
Figure: A: Initial MRI which shows duodenal diverticulum with biliary dilation consistent with Lemmel Syndrome
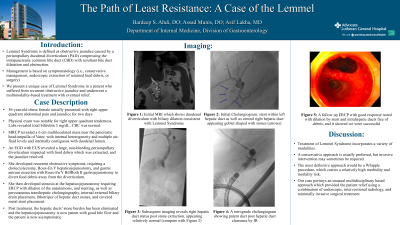
B: Initial Cholangiogram: Stent within left hepatic duct as well as central right hepatic duct appearing goblet shaped with stones (as shown with arrows)
C: Subsequent imaging reveals right hepatic duct status post stone extraction, appearing relatively normal (compare with Image B)
B: Initial Cholangiogram: Stent within left hepatic duct as well as central right hepatic duct appearing goblet shaped with stones (as shown with arrows)
C: Subsequent imaging reveals right hepatic duct status post stone extraction, appearing relatively normal (compare with Image B)
Disclosures:
Hardeep Ahdi indicated no relevant financial relationships.
Assad Munis indicated no relevant financial relationships.
Asif Lakha indicated no relevant financial relationships.
Hardeep S. Ahdi, DO1, Assad Munis, DO2, Asif Lakha, MD2. C0048 - The Path of Least Resistance: A Case of the Lemmel, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
