Back

Poster Session B - Monday Morning
Category: GI Bleeding
B0324 - Secondary Aorto-Esophageal Fistula Caused by Graft Erosion Temporized by Esophageal Stent Placement
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Akshay N. Desai, MD
CMSRU/Cooper University Hospital
Camden, NJ
Presenting Author(s)
Akshay N. Desai, MD1, Ishita Dhawan, MD2, Michael Schwartz, MD2, Krysta Contino, MD1, Adib Chaaya, MD2
1CMSRU/Cooper University Hospital, Camden, NJ; 2Cooper University Hospital, Camden, NJ
Introduction: Aorto-enteric fistulas (AEF) are abnormal connections between the aorta and the gastrointestinal (GI) tract1 which are associated with massive GI hemorrhage and carry a high risk of morbidity3–5. We discuss a case of a cirrhotic patient with a history of varices who presented with hematemesis and was found to have catastrophic bleeding due to an aorto-esophageal fistula.
Case Description/Methods: A 59-year-old male with a history of cirrhosis, esophageal varices, heart failure, and aortic arch aneurysm status post repair, presented with GI bleeding (GIB). Two months prior, the patient had undergone thoracic endovascular aortic aneurysm repair (TEVAR). EGD at the time of that admission for screening showed grade I varices that were not banded. With respect to this admission, he initially presented to an outside institution with hematemesis. He underwent EGD which showed a 1-2 mm esophageal ulcer at 21 cm from the incisors and blood throughout the exam limiting examination and patient was transferred for evaluation.
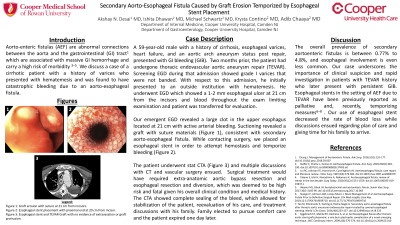
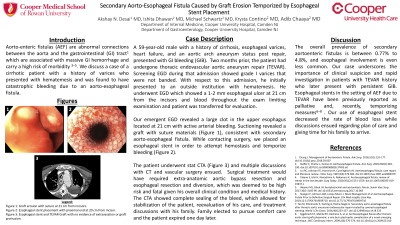
Our emergent EGD revealed a large clot in the upper esophagus located at 21 cm with active arterial bleeding. Suctioning revealed a graft with suture materials (Figure 1), consistent with secondary aorto-esophageal fistula. While contacting surgery, we placed an esophageal stent to attempt hemostasis and temporize bleeding (Figure 2).
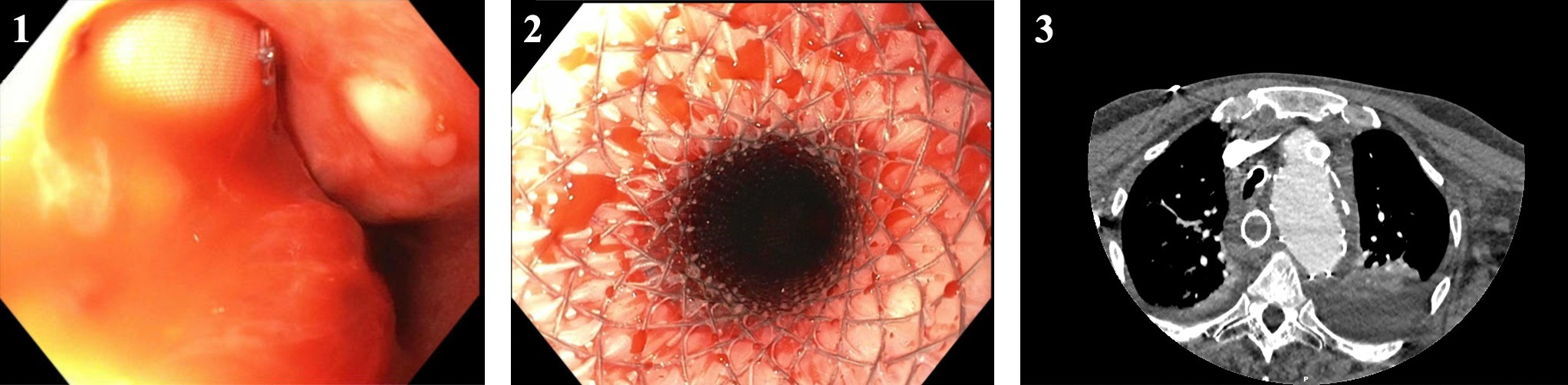
The patient underwent stat CTA (Figure 3) and multiple discussions with CT and vascular surgery ensued. Surgical treatment would have required extra-anatomic aortic bypass resection and esophageal resection and diversion, which was deemed to be high risk and fatal given his overall clinical condition and medical history. The CTA showed complete sealing of the bleed due to stent placement, which allowed for stabilization of the patient, reevaluation of his care, and treatment discussions with his family. Family elected to pursue comfort care and the patient expired one day later.
Discussion: The overall prevalence of secondary aortoenteric fistulas are between 0.77% to 4.8%, and esophageal involvement is even less common. Our case underscores the importance of clinical suspicion and rapid investigation in patients with TEVAR history who later present with persistent GIB. Esophageal stents in the setting of AEF due to TEVAR have been previously reported as palliative and, recently, temporizing measures6–8 . Our use of esophageal stent decreased the rate of blood loss while discussions ensued regarding plan of care and giving time for his family to arrive.
Disclosures:
Akshay N. Desai, MD1, Ishita Dhawan, MD2, Michael Schwartz, MD2, Krysta Contino, MD1, Adib Chaaya, MD2. B0324 - Secondary Aorto-Esophageal Fistula Caused by Graft Erosion Temporized by Esophageal Stent Placement, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1CMSRU/Cooper University Hospital, Camden, NJ; 2Cooper University Hospital, Camden, NJ
Introduction: Aorto-enteric fistulas (AEF) are abnormal connections between the aorta and the gastrointestinal (GI) tract1 which are associated with massive GI hemorrhage and carry a high risk of morbidity3–5. We discuss a case of a cirrhotic patient with a history of varices who presented with hematemesis and was found to have catastrophic bleeding due to an aorto-esophageal fistula.
Case Description/Methods: A 59-year-old male with a history of cirrhosis, esophageal varices, heart failure, and aortic arch aneurysm status post repair, presented with GI bleeding (GIB). Two months prior, the patient had undergone thoracic endovascular aortic aneurysm repair (TEVAR). EGD at the time of that admission for screening showed grade I varices that were not banded. With respect to this admission, he initially presented to an outside institution with hematemesis. He underwent EGD which showed a 1-2 mm esophageal ulcer at 21 cm from the incisors and blood throughout the exam limiting examination and patient was transferred for evaluation.
Our emergent EGD revealed a large clot in the upper esophagus located at 21 cm with active arterial bleeding. Suctioning revealed a graft with suture materials (Figure 1), consistent with secondary aorto-esophageal fistula. While contacting surgery, we placed an esophageal stent to attempt hemostasis and temporize bleeding (Figure 2).
The patient underwent stat CTA (Figure 3) and multiple discussions with CT and vascular surgery ensued. Surgical treatment would have required extra-anatomic aortic bypass resection and esophageal resection and diversion, which was deemed to be high risk and fatal given his overall clinical condition and medical history. The CTA showed complete sealing of the bleed due to stent placement, which allowed for stabilization of the patient, reevaluation of his care, and treatment discussions with his family. Family elected to pursue comfort care and the patient expired one day later.
Discussion: The overall prevalence of secondary aortoenteric fistulas are between 0.77% to 4.8%, and esophageal involvement is even less common. Our case underscores the importance of clinical suspicion and rapid investigation in patients with TEVAR history who later present with persistent GIB. Esophageal stents in the setting of AEF due to TEVAR have been previously reported as palliative and, recently, temporizing measures6–8 . Our use of esophageal stent decreased the rate of blood loss while discussions ensued regarding plan of care and giving time for his family to arrive.
Figure: Figures 1-3: Figure 1 shows graft erosion with suture at 21 cm from incisors. Figure 2 shows esophageal stent placement with proximal end at 20 cm from incisor. Figure 3 shows the presence esophageal stent and TEVAR Graft with no evidence of extravasation or graft protrusion as seen on CTA chest, abdomen, and pelvis.
Disclosures:
Akshay Desai indicated no relevant financial relationships.
Ishita Dhawan indicated no relevant financial relationships.
Michael Schwartz indicated no relevant financial relationships.
Krysta Contino indicated no relevant financial relationships.
Adib Chaaya indicated no relevant financial relationships.
Akshay N. Desai, MD1, Ishita Dhawan, MD2, Michael Schwartz, MD2, Krysta Contino, MD1, Adib Chaaya, MD2. B0324 - Secondary Aorto-Esophageal Fistula Caused by Graft Erosion Temporized by Esophageal Stent Placement, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
