Back
Poster Session B - Monday Morning
Category: Biliary/Pancreas
B0069 - Pancreaticopleural Fistula: A Unique Manifestation of the Sequelae of Pancreatitis
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom

Shil Punatar, DO
Franciscan Health Olympia Fields
Schaumburg, IL
Presenting Author(s)
Shil Punatar, DO1, Ahamed Khalyfa, DO2, Faizan Khan, MD2, Rida Khan, BS3, Zarek Khan, BS4, Fares Hamad, DO5
1Franciscan Health Olympia Fields, Olympia Fields, IL; 2Franciscan Health, Olympia Fields, IL; 3Michigan State University College of Human Medicine, Chicago, IL; 4St. Matthews University of Medicine, Chicago, IL; 5St. Joseph Amita Health, Joliet, IL
Introduction: Acute pancreatitis is a common diagnosis with established guidelines of treatment and patient monitoring. Further known are the potential for common sequelae such as transition to chronic pancreatitis, calcification, and nutritional deficiencies. Lesser known and published in literature are the pleural sequelae of pancreatitis, namely the potential for pancreaticopleural fistulization. Here, we present a case of pancreatitis with pleural fistula formation to shed light on the common presentation, evaluation and treatment methods of this less common diagnosis.
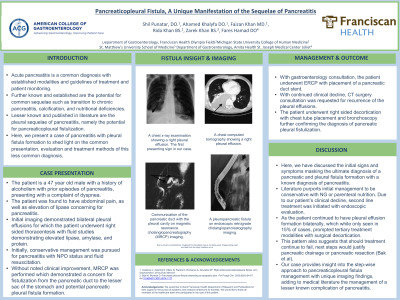
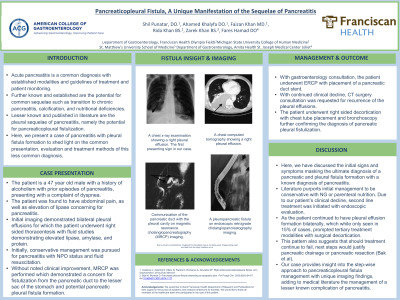
Case Description/Methods: The patient is a 47 year old male with a history of alcoholism with prior episodes of pancreatitis, presenting with a complaint of dyspnea. The patient had abdominal pain, as well as elevation of lipase concerning for pancreatitis. Initial imaging demonstrated bilateral pleural effusions for which the patient underwent right sided thoracentesis with fluid studies demonstrating elevated lipase, amylase, and protein. Initially, conversative management was pursued for pancreatitis with NPO status and fluid resuscitation. Without noted clinical improvement, MRCP was performed which demonstrated a concern for fistulization from the pancreatic duct to the lesser sac of the stomach and potential pancreatic pleural fistula formation. With gastroenterology consultation, the patient underwent ERCP with placement of a pancreatic duct stent. With continued clinical decline, CT surgery consultation was requested for recurrence of the pleural effusions. The patient underwent right sided decortication with chest tube placement and bronchoscopy further confirming the diagnosis of pancreatic pleural fistulization.
Discussion: With this case, we establish the pattern used for treatment of fistulization. Literature purports initial management to be conservative with NG or parenteral nutrition. Due to our patient’s clinical decline, second line treatment was initiated with endoscopic evaluation. As the patient continued to have pleural effusion formation bilaterally, which while only seen in 15% of cases, prompted tertiary treatment modalities with surgical decortication. This pattern also suggests that should treatment continue to fail, next steps would justify pancreatic drainage or pancreatic resection (Bak et al). Our case provides insight into the step-wise approach to pancreaticopleural fistula management with unique imaging findings, adding to medical literature the management of a lesser known complication of pancreatitis.
Disclosures:
Shil Punatar, DO1, Ahamed Khalyfa, DO2, Faizan Khan, MD2, Rida Khan, BS3, Zarek Khan, BS4, Fares Hamad, DO5. B0069 - Pancreaticopleural Fistula: A Unique Manifestation of the Sequelae of Pancreatitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Franciscan Health Olympia Fields, Olympia Fields, IL; 2Franciscan Health, Olympia Fields, IL; 3Michigan State University College of Human Medicine, Chicago, IL; 4St. Matthews University of Medicine, Chicago, IL; 5St. Joseph Amita Health, Joliet, IL
Introduction: Acute pancreatitis is a common diagnosis with established guidelines of treatment and patient monitoring. Further known are the potential for common sequelae such as transition to chronic pancreatitis, calcification, and nutritional deficiencies. Lesser known and published in literature are the pleural sequelae of pancreatitis, namely the potential for pancreaticopleural fistulization. Here, we present a case of pancreatitis with pleural fistula formation to shed light on the common presentation, evaluation and treatment methods of this less common diagnosis.
Case Description/Methods: The patient is a 47 year old male with a history of alcoholism with prior episodes of pancreatitis, presenting with a complaint of dyspnea. The patient had abdominal pain, as well as elevation of lipase concerning for pancreatitis. Initial imaging demonstrated bilateral pleural effusions for which the patient underwent right sided thoracentesis with fluid studies demonstrating elevated lipase, amylase, and protein. Initially, conversative management was pursued for pancreatitis with NPO status and fluid resuscitation. Without noted clinical improvement, MRCP was performed which demonstrated a concern for fistulization from the pancreatic duct to the lesser sac of the stomach and potential pancreatic pleural fistula formation. With gastroenterology consultation, the patient underwent ERCP with placement of a pancreatic duct stent. With continued clinical decline, CT surgery consultation was requested for recurrence of the pleural effusions. The patient underwent right sided decortication with chest tube placement and bronchoscopy further confirming the diagnosis of pancreatic pleural fistulization.
Discussion: With this case, we establish the pattern used for treatment of fistulization. Literature purports initial management to be conservative with NG or parenteral nutrition. Due to our patient’s clinical decline, second line treatment was initiated with endoscopic evaluation. As the patient continued to have pleural effusion formation bilaterally, which while only seen in 15% of cases, prompted tertiary treatment modalities with surgical decortication. This pattern also suggests that should treatment continue to fail, next steps would justify pancreatic drainage or pancreatic resection (Bak et al). Our case provides insight into the step-wise approach to pancreaticopleural fistula management with unique imaging findings, adding to medical literature the management of a lesser known complication of pancreatitis.
Disclosures:
Shil Punatar indicated no relevant financial relationships.
Ahamed Khalyfa indicated no relevant financial relationships.
Faizan Khan indicated no relevant financial relationships.
Rida Khan indicated no relevant financial relationships.
Zarek Khan indicated no relevant financial relationships.
Fares Hamad indicated no relevant financial relationships.
Shil Punatar, DO1, Ahamed Khalyfa, DO2, Faizan Khan, MD2, Rida Khan, BS3, Zarek Khan, BS4, Fares Hamad, DO5. B0069 - Pancreaticopleural Fistula: A Unique Manifestation of the Sequelae of Pancreatitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
