Back

Poster Session C - Monday Afternoon
Category: Colon
C0101 - Trends and Disparities in Outcomes of Hospitalizations With Clostridioides difficile, Infection: A Decade-Long Analysis of the Nationwide Inpatient Sample
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Pius E. Ojemolon, MD
John H. Stroger, Jr. Hospital of Cook County
Chicago, IL
Presenting Author(s)
Pius E. Ojemolon, MD1, Robert Kwei-Nsoro, MD1, Hisham Laswi, MD1, Ebehiwele Ebhohon, MD2, Hafeez Shaka, MBBS1
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2Lincoln Medical Center, Bronx, NY
Introduction: Clostridioides difficile infection (CDI) is the most frequently reported nosocomial infection. There is a paucity of research on the impact of sociodemographic indices on CDI hospitalization outcomes. This study aimed to describe epidemiologic trends and effects of sociodemographic disparities on outcomes among CDI hospitalizations over a decade.
Methods: We queried Nationwide Inpatient Sample (NIS) databases from 2010 to 2019, identified hospitalizations with CDI, and excluded those of patients less than 18 years. We obtained the incidence and admission rate of CDI per 100,000 adult hospitalizations for each year. We analyzed trends in mortality rate, mean length of hospital stay (LOS), and mean total hospital charge (THC). We highlighted disparities in outcomes stratified by sex, race, and mean household income (MHOI) quartile. We used multivariable regression analysis to obtain trends in incidence and admission rates, mortality, LOS, and THC adjusted for age categories, sex, and race. We used Joinpoint regression analysis to obtain trends in adjusted rates. The threshold for statistical significance was set at 0.05.
Results: Of the 305 million hospitalizations included in our study, over 3.3 million were complicated by CDI, with 1.01 million principal admissions for CDI. There was an average annual percentage change (AAPC) of -2% reduction in adjusted CDI incidence and AAPC for CDI admissions was -3.2%. Joinpoint regression analysis showed an increased adjusted CDI admission rate from 2010 to 2012 (annual percentage change [APC] = 4.15%), with a subsequent decrease from 2012 to 2016 (APC = -2.17%), and 2016 to 2019 (APC = -9.87%).
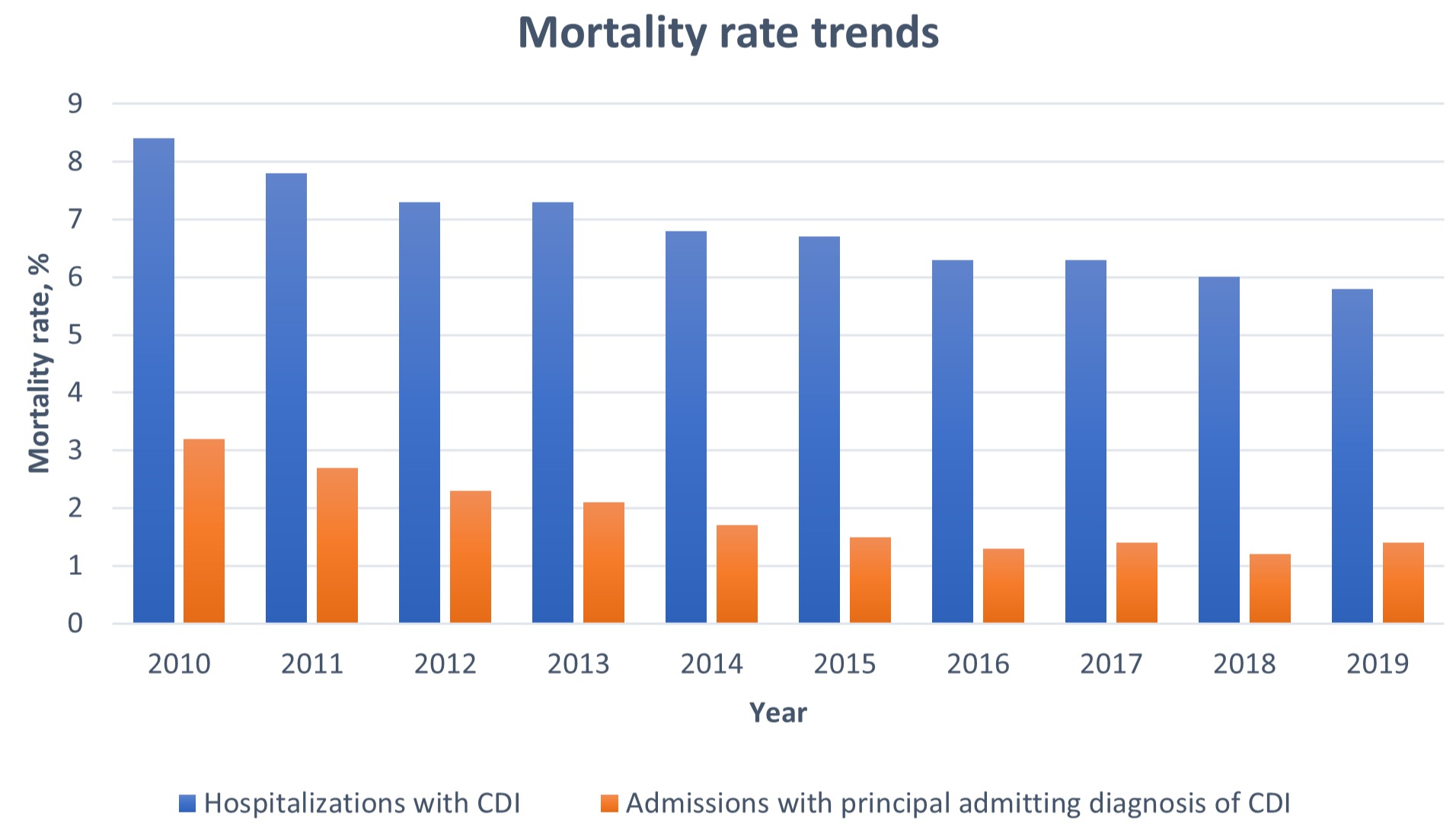
Among primary admissions for CDI, mortality rate decreased from 3.2% in 2010 to 1.4% in 2019. The AAPC for adjusted mortality rate was -10.2%. Mean LOS reduced from 6.6 to 5.3 days while mean THC increased from US$40,593 to US$42,934 between 2010 and 2019. Females had a 21% decrease in adjusted odds of mortality compared to males (all p-trends < 0.001). Mortality rates showed a steady decline among Whites over the study period. Mean LOS trends were similar across racial subgroups. Mortality rates, mean LOS and mean THC followed similar trends in hospitalizations among low and high MHOI quartiles.
Discussion: Outcomes of CDI hospitalizations improved over the studied decade but were consistently better in females than males, with better improvements among Whites than Blacks or Hispanics. Further studies are needed to elucidate the reasons for these findings.
Disclosures:
Pius E. Ojemolon, MD1, Robert Kwei-Nsoro, MD1, Hisham Laswi, MD1, Ebehiwele Ebhohon, MD2, Hafeez Shaka, MBBS1. C0101 - Trends and Disparities in Outcomes of Hospitalizations With Clostridioides difficile, Infection: A Decade-Long Analysis of the Nationwide Inpatient Sample, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2Lincoln Medical Center, Bronx, NY
Introduction: Clostridioides difficile infection (CDI) is the most frequently reported nosocomial infection. There is a paucity of research on the impact of sociodemographic indices on CDI hospitalization outcomes. This study aimed to describe epidemiologic trends and effects of sociodemographic disparities on outcomes among CDI hospitalizations over a decade.
Methods: We queried Nationwide Inpatient Sample (NIS) databases from 2010 to 2019, identified hospitalizations with CDI, and excluded those of patients less than 18 years. We obtained the incidence and admission rate of CDI per 100,000 adult hospitalizations for each year. We analyzed trends in mortality rate, mean length of hospital stay (LOS), and mean total hospital charge (THC). We highlighted disparities in outcomes stratified by sex, race, and mean household income (MHOI) quartile. We used multivariable regression analysis to obtain trends in incidence and admission rates, mortality, LOS, and THC adjusted for age categories, sex, and race. We used Joinpoint regression analysis to obtain trends in adjusted rates. The threshold for statistical significance was set at 0.05.
Results: Of the 305 million hospitalizations included in our study, over 3.3 million were complicated by CDI, with 1.01 million principal admissions for CDI. There was an average annual percentage change (AAPC) of -2% reduction in adjusted CDI incidence and AAPC for CDI admissions was -3.2%. Joinpoint regression analysis showed an increased adjusted CDI admission rate from 2010 to 2012 (annual percentage change [APC] = 4.15%), with a subsequent decrease from 2012 to 2016 (APC = -2.17%), and 2016 to 2019 (APC = -9.87%).
Among primary admissions for CDI, mortality rate decreased from 3.2% in 2010 to 1.4% in 2019. The AAPC for adjusted mortality rate was -10.2%. Mean LOS reduced from 6.6 to 5.3 days while mean THC increased from US$40,593 to US$42,934 between 2010 and 2019. Females had a 21% decrease in adjusted odds of mortality compared to males (all p-trends < 0.001). Mortality rates showed a steady decline among Whites over the study period. Mean LOS trends were similar across racial subgroups. Mortality rates, mean LOS and mean THC followed similar trends in hospitalizations among low and high MHOI quartiles.
Discussion: Outcomes of CDI hospitalizations improved over the studied decade but were consistently better in females than males, with better improvements among Whites than Blacks or Hispanics. Further studies are needed to elucidate the reasons for these findings.
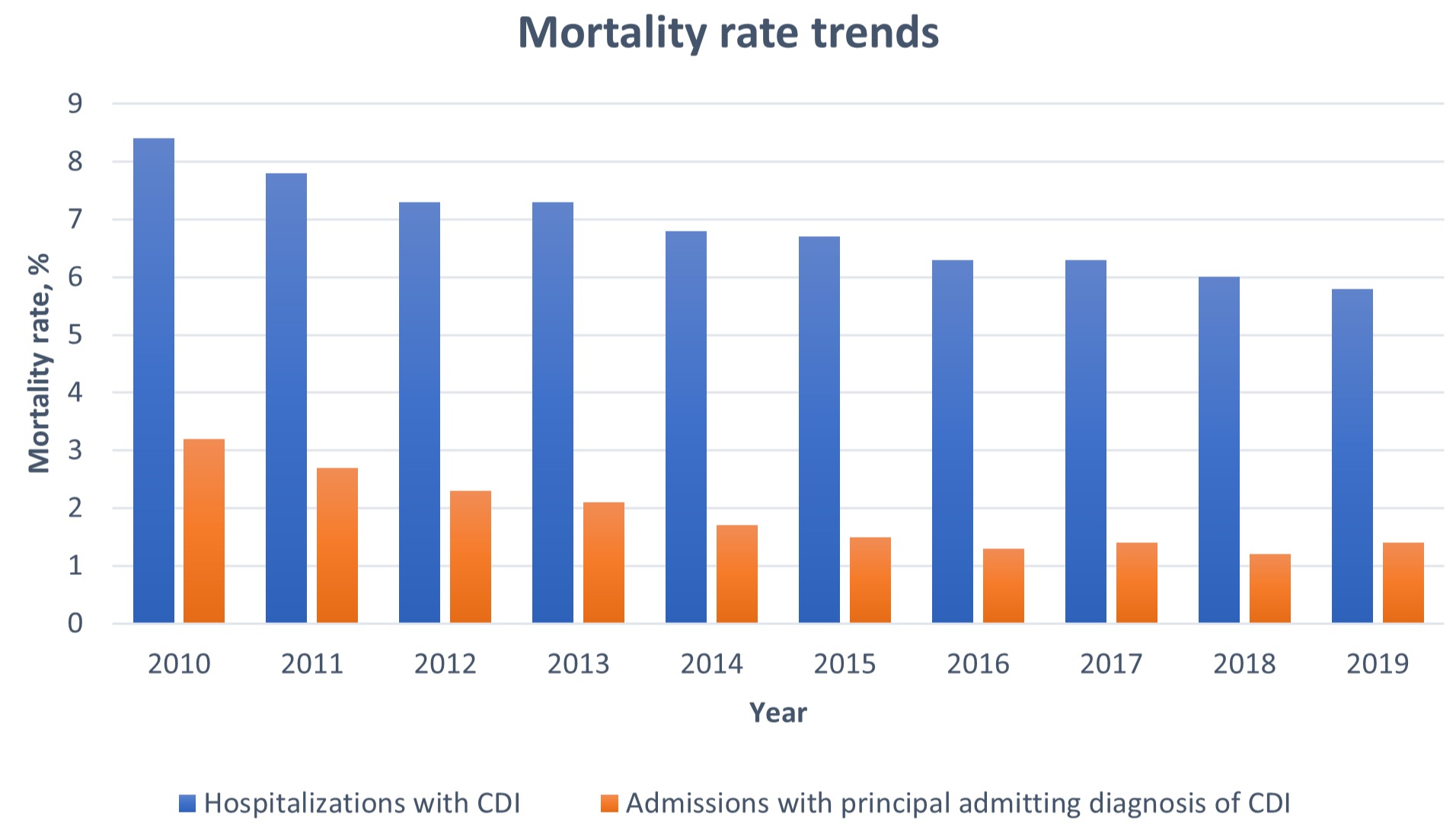
Figure: Figure 1: Trends in mortality rates among hospitalizations with CDI and admissions with principal admitting diagnosis of CDI
Disclosures:
Pius Ojemolon indicated no relevant financial relationships.
Robert Kwei-Nsoro indicated no relevant financial relationships.
Hisham Laswi indicated no relevant financial relationships.
Ebehiwele Ebhohon indicated no relevant financial relationships.
Hafeez Shaka indicated no relevant financial relationships.
Pius E. Ojemolon, MD1, Robert Kwei-Nsoro, MD1, Hisham Laswi, MD1, Ebehiwele Ebhohon, MD2, Hafeez Shaka, MBBS1. C0101 - Trends and Disparities in Outcomes of Hospitalizations With Clostridioides difficile, Infection: A Decade-Long Analysis of the Nationwide Inpatient Sample, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
