Back


Poster Session C - Monday Afternoon
Category: Colon
C0148 - Mucosal Schwann Cell Hamartoma: A Benign but Obscure Finding
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Has Audio

Jason J. John, MD
University of South Florida Health
Tampa, FL
Presenting Author(s)
Jason J. John, MD1, Jennifer L. Reed, MD2, Wojciech Blonski, MD, PhD2
1University of South Florida Health, Tampa, FL; 2James A. Haley VA Hospital, Tampa, FL
Introduction: Mucosal Schwann Cell Hamartoma (MSCH) is a rare entity with few case reports present in literature. While harboring no malignant potential, it is more commonly found in the elderly. We report a case of a 69-year-old male patient found to have a MSCH.
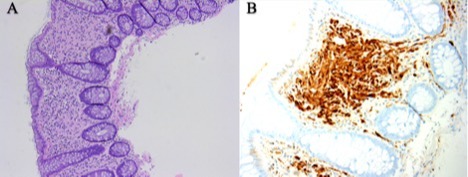
Case Description/Methods: A 69-year-old African American male with no history of gastrointestinal disease and no family history of neuronal lesion presented for a follow up colonoscopy. Previous colonoscopy in 2017 showed 6 subcentimeter sessile polyps, one of which was a 5 mm polyp in the sigmoid colon, all removed by cold snare polypectomies. Histology of this polyp was consistent with MSCH (Figure 1), with the other polyps showing tubular adenomas (TA). Immunohistochemical (IHC) stains were positive for S100, and negative for CD68 and SMA further supporting the diagnosis. The patient was otherwise asymptomatic. The follow up colonoscopy five years later revealed 6 subcentimeter sessile polyps with one being a 5 mm polyp in the sigmoid colon. Histology of this polyp revealed MSCH and the other polyps revealed TA.
Discussion: MSCH of the sigmoid colon is a rare condition that is usually an incidental finding on colonoscopy. MSCH is a benign mesenchymal nerve sheath tumor originating from Schwann cells, arising in the lamina propria of the colon. They are most commonly seen in the sigmoid colon and are detected as small polyps anywhere between 1 – 8 mm. There is no association with any inherited disorder. Most patients present asymptomatically, however, when symptomatic, patients can present with diarrhea, abdominal pain, bleeding, or constipation. Because of its rarity, the significance of the finding is not clear. Currently, there are no guidelines for surveillance colonoscopy for MSCH. It is important to accurately identify these hamartomas, as they can mimic malignant lesions or lesions with malignant potential such as colonic leiomyoma, gastrointestinal stromal tumor (GIST), GI schwannomas and neurofibromas. Diagnosis is dependent on histological features and IHC pattern. On histology, hamartomas show proliferation of spindle cells in the lamina propria separating the crypt architecture. Strong positivity for S100, and negative CD68 and SMA is suggestive of neural origin and prove Schwann cell phenotype. There have been no reports of malignant transformation in literature. Awareness of this entity could prevent additional endoscopies for patients and decrease healthcare costs from unnecessary surveillance and treatments.
Disclosures:
Jason J. John, MD1, Jennifer L. Reed, MD2, Wojciech Blonski, MD, PhD2. C0148 - Mucosal Schwann Cell Hamartoma: A Benign but Obscure Finding, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of South Florida Health, Tampa, FL; 2James A. Haley VA Hospital, Tampa, FL
Introduction: Mucosal Schwann Cell Hamartoma (MSCH) is a rare entity with few case reports present in literature. While harboring no malignant potential, it is more commonly found in the elderly. We report a case of a 69-year-old male patient found to have a MSCH.
Case Description/Methods: A 69-year-old African American male with no history of gastrointestinal disease and no family history of neuronal lesion presented for a follow up colonoscopy. Previous colonoscopy in 2017 showed 6 subcentimeter sessile polyps, one of which was a 5 mm polyp in the sigmoid colon, all removed by cold snare polypectomies. Histology of this polyp was consistent with MSCH (Figure 1), with the other polyps showing tubular adenomas (TA). Immunohistochemical (IHC) stains were positive for S100, and negative for CD68 and SMA further supporting the diagnosis. The patient was otherwise asymptomatic. The follow up colonoscopy five years later revealed 6 subcentimeter sessile polyps with one being a 5 mm polyp in the sigmoid colon. Histology of this polyp revealed MSCH and the other polyps revealed TA.
Discussion: MSCH of the sigmoid colon is a rare condition that is usually an incidental finding on colonoscopy. MSCH is a benign mesenchymal nerve sheath tumor originating from Schwann cells, arising in the lamina propria of the colon. They are most commonly seen in the sigmoid colon and are detected as small polyps anywhere between 1 – 8 mm. There is no association with any inherited disorder. Most patients present asymptomatically, however, when symptomatic, patients can present with diarrhea, abdominal pain, bleeding, or constipation. Because of its rarity, the significance of the finding is not clear. Currently, there are no guidelines for surveillance colonoscopy for MSCH. It is important to accurately identify these hamartomas, as they can mimic malignant lesions or lesions with malignant potential such as colonic leiomyoma, gastrointestinal stromal tumor (GIST), GI schwannomas and neurofibromas. Diagnosis is dependent on histological features and IHC pattern. On histology, hamartomas show proliferation of spindle cells in the lamina propria separating the crypt architecture. Strong positivity for S100, and negative CD68 and SMA is suggestive of neural origin and prove Schwann cell phenotype. There have been no reports of malignant transformation in literature. Awareness of this entity could prevent additional endoscopies for patients and decrease healthcare costs from unnecessary surveillance and treatments.
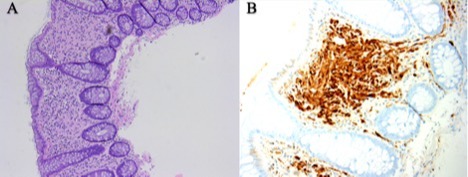
Figure: Figure 1: A. H&E stain of mucosal proliferation in the lamina propria. B. S100+ staining (brown)
Disclosures:
Jason John indicated no relevant financial relationships.
Jennifer Reed indicated no relevant financial relationships.
Wojciech Blonski indicated no relevant financial relationships.
Jason J. John, MD1, Jennifer L. Reed, MD2, Wojciech Blonski, MD, PhD2. C0148 - Mucosal Schwann Cell Hamartoma: A Benign but Obscure Finding, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
