Back

Poster Session A - Sunday Afternoon
Category: Biliary/Pancreas
A0008 - The Impact of Early Detection of Malignant Biliary Obstruction by Endoscopic Ultrasound on Clinical Outcomes After Surgical Resection
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Vitchapong Prasitsumrit, MD
Siriraj Hospital
Bangkok, Krung Thep, Thailand
Presenting Author(s)
Vitchapong Prasitsumrit, MD1, Nonthalee Pausawasdi, MD1, Yongyut Sirivatanaukson, MD, PhD1, Phunchai Charatchareonwitthaya, MD1, Kesinee Yingcharoen, MD2, Tuangporn Siriphiphatcharoen, MD1
1Siriraj Hospital, Bangkok, Krung Thep, Thailand; 2Chulabhorn Hospital, Bangkok, Krung Thep, Thailand
Introduction: Computerized tomography (CT) scan and endoscopic ultrasound (EUS) are the main diagnostic tools for detecting periampullary cancers. EUS allows the detection of small tumors missed by CT scan in patients presenting with bile duct obstruction. However, the impact of EUS in diagnosing small tumors on clinical outcomes is yet to be explored. This study aimed to compare the tumor recurrence rate and survival benefit of patients following pancreaticoduodenectomy (PD) for periampullary cancers detected by abdominal CT vs. EUS after negative CT.
Methods: A retrospective review of the EUS and surgery database from 2009 to 2021. The patients who underwent PD for periampullary cancer were recruited. The patients were divided into CT-guided surgery group (CT group) and EUS-guided surgery group (EUS group). The clinical outcomes between the 2 groups were compared.
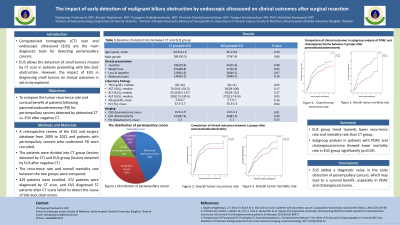
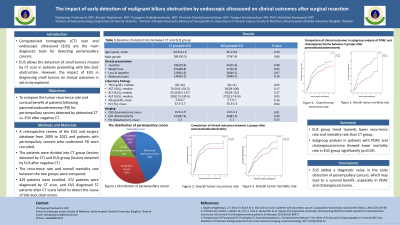
Results: 429 patients were enrolled. 372 patients were diagnosed by CT scan, and EUS diagnosed 57 patients after CT scans failed to detect the cause of bile duct obstruction. The mean age was 64.7+ 11.9 years. The common presentations included jaundice (79.0 %) and weight loss (66.9%). Pancreatic adenocarcinoma (PDAC) was the most common cancer (43.6%), followed by ampullary cancer (32.4%), distal cholangiocarcinoma (14.2%), and duodenal cancer (9.8%). There were no differences in patient demographics between the two groups regarding age, gender, and underlying diseases. Patients in the CT group had higher serum bilirubin (p=0.025), higher serum alkaline phosphatase (p=0.047), lower serum hematocrit (p=0.043), and larger CBD diameter (p=0.005) compared to the EUS group. The T and M staging were not different between the two groups; however, the percentage of patients with nodal metastasis was higher in the CT group (p=0.014). Multivariate analysis showed a trend towards higher recurrence and 5-year mortality rate in the CT group with odds ratios (OR) of 1.33 (95% CI, 0.82-2.13) and 1.43 (95% CI, 0.84-2.42), respectively. Subgroup analysis of PDAC and cholangiocarcinoma demonstrated a significantly higher mortality rate of patients in the CT group with an OR of 2.82 (95% CI, 1.14-6.99, p=0.026) and a trend toward a higher recurrence rate after surgery with the OR of 1.45 (95% CI, 0.80-2.66) compared to the EUS group.
Discussion: EUS added a diagnostic value in the early detection of periampullary cancers, which may lead to a survival benefit, especially in PDAC and cholangiocarcinoma.
Disclosures:
Vitchapong Prasitsumrit, MD1, Nonthalee Pausawasdi, MD1, Yongyut Sirivatanaukson, MD, PhD1, Phunchai Charatchareonwitthaya, MD1, Kesinee Yingcharoen, MD2, Tuangporn Siriphiphatcharoen, MD1. A0008 - The Impact of Early Detection of Malignant Biliary Obstruction by Endoscopic Ultrasound on Clinical Outcomes After Surgical Resection, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Siriraj Hospital, Bangkok, Krung Thep, Thailand; 2Chulabhorn Hospital, Bangkok, Krung Thep, Thailand
Introduction: Computerized tomography (CT) scan and endoscopic ultrasound (EUS) are the main diagnostic tools for detecting periampullary cancers. EUS allows the detection of small tumors missed by CT scan in patients presenting with bile duct obstruction. However, the impact of EUS in diagnosing small tumors on clinical outcomes is yet to be explored. This study aimed to compare the tumor recurrence rate and survival benefit of patients following pancreaticoduodenectomy (PD) for periampullary cancers detected by abdominal CT vs. EUS after negative CT.
Methods: A retrospective review of the EUS and surgery database from 2009 to 2021. The patients who underwent PD for periampullary cancer were recruited. The patients were divided into CT-guided surgery group (CT group) and EUS-guided surgery group (EUS group). The clinical outcomes between the 2 groups were compared.
Results: 429 patients were enrolled. 372 patients were diagnosed by CT scan, and EUS diagnosed 57 patients after CT scans failed to detect the cause of bile duct obstruction. The mean age was 64.7+ 11.9 years. The common presentations included jaundice (79.0 %) and weight loss (66.9%). Pancreatic adenocarcinoma (PDAC) was the most common cancer (43.6%), followed by ampullary cancer (32.4%), distal cholangiocarcinoma (14.2%), and duodenal cancer (9.8%). There were no differences in patient demographics between the two groups regarding age, gender, and underlying diseases. Patients in the CT group had higher serum bilirubin (p=0.025), higher serum alkaline phosphatase (p=0.047), lower serum hematocrit (p=0.043), and larger CBD diameter (p=0.005) compared to the EUS group. The T and M staging were not different between the two groups; however, the percentage of patients with nodal metastasis was higher in the CT group (p=0.014). Multivariate analysis showed a trend towards higher recurrence and 5-year mortality rate in the CT group with odds ratios (OR) of 1.33 (95% CI, 0.82-2.13) and 1.43 (95% CI, 0.84-2.42), respectively. Subgroup analysis of PDAC and cholangiocarcinoma demonstrated a significantly higher mortality rate of patients in the CT group with an OR of 2.82 (95% CI, 1.14-6.99, p=0.026) and a trend toward a higher recurrence rate after surgery with the OR of 1.45 (95% CI, 0.80-2.66) compared to the EUS group.
Discussion: EUS added a diagnostic value in the early detection of periampullary cancers, which may lead to a survival benefit, especially in PDAC and cholangiocarcinoma.
Disclosures:
Vitchapong Prasitsumrit indicated no relevant financial relationships.
Nonthalee Pausawasdi indicated no relevant financial relationships.
Yongyut Sirivatanaukson indicated no relevant financial relationships.
Phunchai Charatchareonwitthaya indicated no relevant financial relationships.
Kesinee Yingcharoen indicated no relevant financial relationships.
Tuangporn Siriphiphatcharoen indicated no relevant financial relationships.
Vitchapong Prasitsumrit, MD1, Nonthalee Pausawasdi, MD1, Yongyut Sirivatanaukson, MD, PhD1, Phunchai Charatchareonwitthaya, MD1, Kesinee Yingcharoen, MD2, Tuangporn Siriphiphatcharoen, MD1. A0008 - The Impact of Early Detection of Malignant Biliary Obstruction by Endoscopic Ultrasound on Clinical Outcomes After Surgical Resection, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
