Back
Poster Session B - Monday Morning
Category: Esophagus
B0241 - The First Case of Water Immersion Endoscopy in the Definitive Diagnosis of Atrio: Esophageal Fistula
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
- FS
Farah Shirazi, MD
California Pacific Medical Center
San Francisco, California
Presenting Author(s)
Farah Shirazi, MD1, Mona Rezapour, MD2, Mimi Lin, MD1
1California Pacific Medical Center, San Francisco, CA; 2University of California Los Angeles, Los Angeles, CA
Introduction: Atrial fibrillation (AF) is the most common heart rhythm disorder with estimated global prevalence of 33.5 million. Catheter ablation is the treatment modality of choice for refractory AF. Atrio-esophageal fistula (AEF) is a serious complication of catheter ablation. Diagnosis is critical to the management of AEF, and includes computed tomography of the chest, esophagram and esophagogastroduodenoscopy (EGD). Prompt diagnosis of AEF is essential for survival.
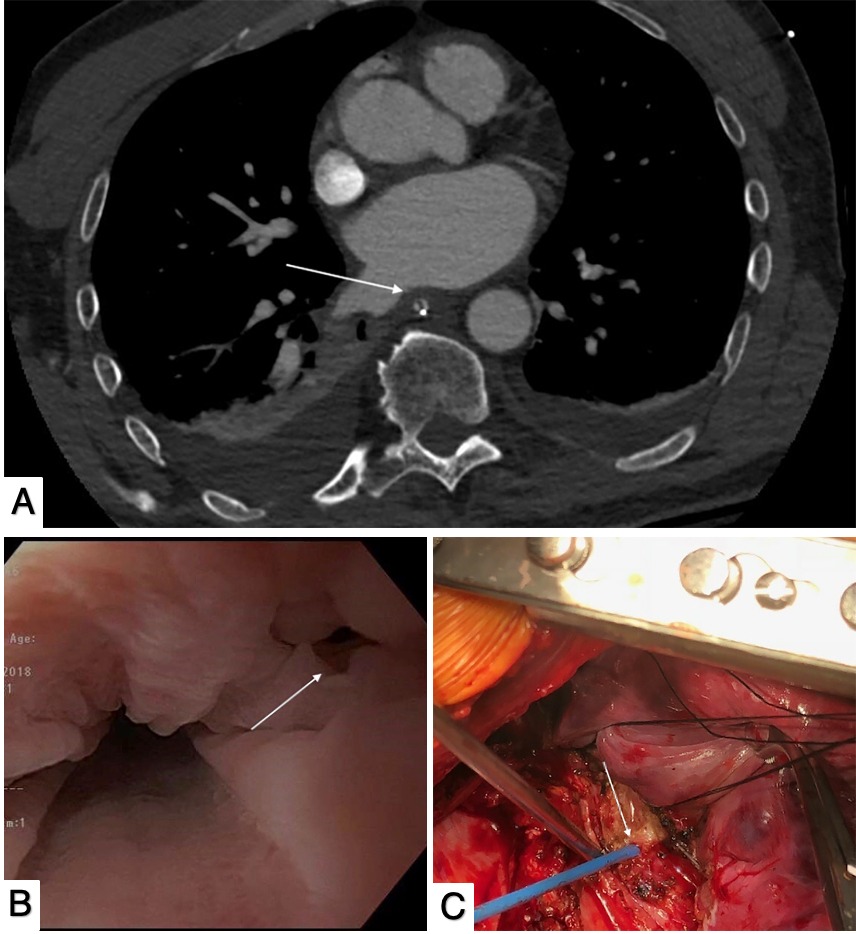
Case Description/Methods: A 56-year-old male with AF presented with fever, fatigue and bilateral leg weakness. Twenty days prior to presentation he underwent pulmonary vein isolation radiofrequency ablation and discharged the following day. Upon re-presentation his vitals were notable for fever and tachycardia. Labs revealed a normal white count and hemoglobin, and elevated lactate and troponin. One hour after arrival he developed complex focal seizure and AF with rapid ventricular rate followed by respiratory decompensation requiring intubation. His blood cultures revealed Streptococcus mitis and Gemella haemolysans. His MRI disclosed numerous bilateral emboli concerning for endocarditis, however TEE did not reveal any valvular vegetation, thus proposing AEF as a possible complication accounting for the emboli. CT chest angiogram revealed subtle irregularity along the posterior wall of the left atrium (figure1A), but did not provide conclusive evidence to warrant high-risk cardiothoracic surgery. Water immersion EGD was performed to diagnose and localize the fistula, revealing esophageal defect in the proximal esophagus with movement of non-bloody debris through the tract (figure 1B). One hemostatic clip was placed near the tract to assist with localization for surgical closure. The following day the patient underwent right thoracotomy with placement of intercostal muscle flap to fistula (Figure 1C).
Discussion: AEF is a rare complication of radiofrequency ablation therapy for AF. High mortality rate is primarily attributed to major cerebrovascular morbidity from septic thrombi. Currently there is no effective modality to visualize AEF safely and reliably. Water immersion colonoscopy allows for completion of difficult colonoscopies, decreased insertion pain, and increased adenoma-detection rates. This technique was applied to identify the AEF. Water immersion EGD is an important modality that can confidently be considered within the diagnostic armamentarium of gastroenterologists to ensure safe and rapid diagnosis and treatment of AEF.
Disclosures:
Farah Shirazi, MD1, Mona Rezapour, MD2, Mimi Lin, MD1. B0241 - The First Case of Water Immersion Endoscopy in the Definitive Diagnosis of Atrio: Esophageal Fistula, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1California Pacific Medical Center, San Francisco, CA; 2University of California Los Angeles, Los Angeles, CA
Introduction: Atrial fibrillation (AF) is the most common heart rhythm disorder with estimated global prevalence of 33.5 million. Catheter ablation is the treatment modality of choice for refractory AF. Atrio-esophageal fistula (AEF) is a serious complication of catheter ablation. Diagnosis is critical to the management of AEF, and includes computed tomography of the chest, esophagram and esophagogastroduodenoscopy (EGD). Prompt diagnosis of AEF is essential for survival.
Case Description/Methods: A 56-year-old male with AF presented with fever, fatigue and bilateral leg weakness. Twenty days prior to presentation he underwent pulmonary vein isolation radiofrequency ablation and discharged the following day. Upon re-presentation his vitals were notable for fever and tachycardia. Labs revealed a normal white count and hemoglobin, and elevated lactate and troponin. One hour after arrival he developed complex focal seizure and AF with rapid ventricular rate followed by respiratory decompensation requiring intubation. His blood cultures revealed Streptococcus mitis and Gemella haemolysans. His MRI disclosed numerous bilateral emboli concerning for endocarditis, however TEE did not reveal any valvular vegetation, thus proposing AEF as a possible complication accounting for the emboli. CT chest angiogram revealed subtle irregularity along the posterior wall of the left atrium (figure1A), but did not provide conclusive evidence to warrant high-risk cardiothoracic surgery. Water immersion EGD was performed to diagnose and localize the fistula, revealing esophageal defect in the proximal esophagus with movement of non-bloody debris through the tract (figure 1B). One hemostatic clip was placed near the tract to assist with localization for surgical closure. The following day the patient underwent right thoracotomy with placement of intercostal muscle flap to fistula (Figure 1C).
Discussion: AEF is a rare complication of radiofrequency ablation therapy for AF. High mortality rate is primarily attributed to major cerebrovascular morbidity from septic thrombi. Currently there is no effective modality to visualize AEF safely and reliably. Water immersion colonoscopy allows for completion of difficult colonoscopies, decreased insertion pain, and increased adenoma-detection rates. This technique was applied to identify the AEF. Water immersion EGD is an important modality that can confidently be considered within the diagnostic armamentarium of gastroenterologists to ensure safe and rapid diagnosis and treatment of AEF.
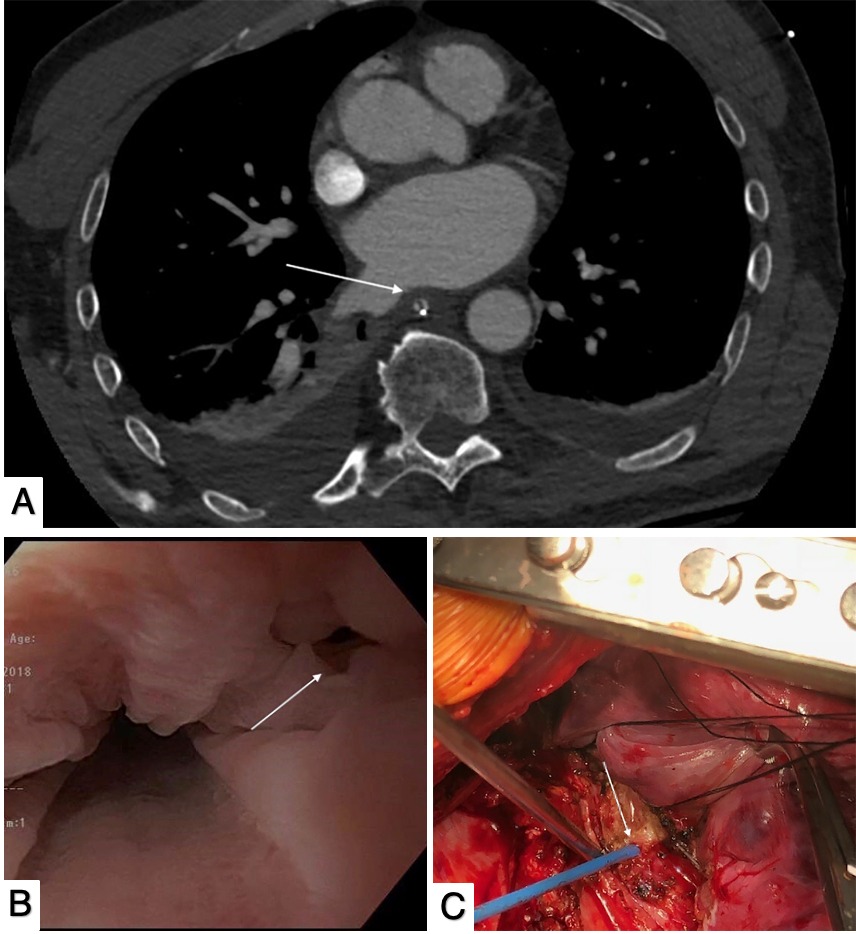
Figure: Figure 1: (A) Illustrates a subtle contour abnormality involving the posterior wall of the left atrium (arrow) concerning for AEF (B) Water immersion endoscopy illustrating 3mm defect (arrow) in the wall of the esophagus (C) Underwent right thoracotomy to access AEF. This image highlights 3mm fistula site (arrow) that is approximated to be at the midpoint of the atrium.
Disclosures:
Farah Shirazi indicated no relevant financial relationships.
Mona Rezapour: Abbvie – Speakers Bureau. BMS – Advisory Committee/Board Member. Takeda – Speakers Bureau.
Mimi Lin indicated no relevant financial relationships.
Farah Shirazi, MD1, Mona Rezapour, MD2, Mimi Lin, MD1. B0241 - The First Case of Water Immersion Endoscopy in the Definitive Diagnosis of Atrio: Esophageal Fistula, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
