Back
Poster Session B - Monday Morning
Category: GI Bleeding
B0340 - A Case of Capecitabine-Induced Gastrointestinal Hemorrhage
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
- SG
Sanda Gomez-Paz, MD
Nassau University Medical Center
East Meadow, NY
Presenting Author(s)
Sandra Gomez-Paz, MD, Kevin Yeroushalmi, MD, Jiten Desai, MD, Deepthi Kagolanu, MD, Kaleem Rizvon, , Nausheer Khan, MD, Paul Mustacchia, MD, MBA
Nassau University Medical Center, East Meadow, NY
Introduction: Capecitabine is a common agent utilized in adjuvant chemotherapy for breast, esophageal and colorectal cancers. Capecitabine- induced terminal ileitis or ileocolitis leading to severe gastrointestinal bleed is rare but potentially life-threatening, requiring early intervention and timely recognition of associated symptoms. We present the case of a patient with capecitabine-induced ileocolitis who presented with persistent high-grade bloody diarrhea.
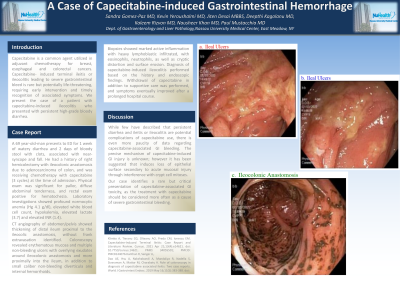
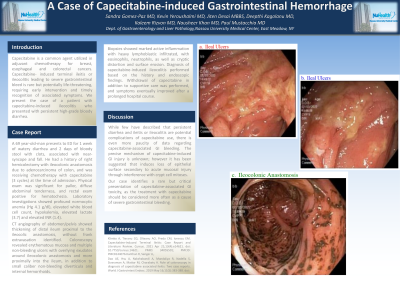
Case Description/Methods: A 69 year-old-man presents to ED for 1 week of watery diarrhea and 2 days of bloody stool with clots, associated with near-syncope and fall. He had a history of right hemicolectomy with ileocolonic anastomosis due to adenocarcinoma of colon, and was receiving chemotherapy with capecitabine (3 cycles) at the time of admission. Physical exam was significant for pallor, diffuse abdominal tenderness, and rectal exam positive for hematochezia. Laboratory investigations showed profound normocytic anemia (Hg 4.1 g/dl), elevated white blood cell count, hypokalemia, elevated lactate (3.7) and elevated INR (1.4). CT angiography of abdomen/pelvis showed thickening of distal ileum proximal to the ileocolic anastomosis, without frank extravasation identified. Colonoscopy revealed erythematous mucosa and multiple non-bleeding ulcers with overlying exudates around ileocolonic anastomosis and more proximally into the ileum, in addition to small caliber non-bleeding diverticula and internal hemorrhoids. Biopsies showed marked active inflammation with heavy lymphoblastic infiltrated, with eosinophils, neutrophils, as well as cryptic distortion and surface erosion. Diagnosis of capecitabine-induced ileocolitis performed based on the history and endoscopic findings. Withdrawal of capecitabine in addition to supportive care was performed, and symptoms eventually improved after a prolonged hospital course.
Discussion: While few have described that persistent diarrhea and ileitis or ileocolitis are potential complications of capecitabine use, there is even more paucity of data regarding capecitabine-associated GI bleeding. The precise mechanism of capecitabine-induced GI injury is unknown; however it has been suggested that induces loss of epithelial surface secondary to acute mucosal injury through interference with crypt cell mitoses. Our case identifies a rare but critical presentation of capecitabine-associated GI toxicity, as the treatment with capecitabine should be considered more often as a cause of severe gastrointestinal bleeding.
Disclosures:
Sandra Gomez-Paz, MD, Kevin Yeroushalmi, MD, Jiten Desai, MD, Deepthi Kagolanu, MD, Kaleem Rizvon, , Nausheer Khan, MD, Paul Mustacchia, MD, MBA. B0340 - A Case of Capecitabine-Induced Gastrointestinal Hemorrhage, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Nassau University Medical Center, East Meadow, NY
Introduction: Capecitabine is a common agent utilized in adjuvant chemotherapy for breast, esophageal and colorectal cancers. Capecitabine- induced terminal ileitis or ileocolitis leading to severe gastrointestinal bleed is rare but potentially life-threatening, requiring early intervention and timely recognition of associated symptoms. We present the case of a patient with capecitabine-induced ileocolitis who presented with persistent high-grade bloody diarrhea.
Case Description/Methods: A 69 year-old-man presents to ED for 1 week of watery diarrhea and 2 days of bloody stool with clots, associated with near-syncope and fall. He had a history of right hemicolectomy with ileocolonic anastomosis due to adenocarcinoma of colon, and was receiving chemotherapy with capecitabine (3 cycles) at the time of admission. Physical exam was significant for pallor, diffuse abdominal tenderness, and rectal exam positive for hematochezia. Laboratory investigations showed profound normocytic anemia (Hg 4.1 g/dl), elevated white blood cell count, hypokalemia, elevated lactate (3.7) and elevated INR (1.4). CT angiography of abdomen/pelvis showed thickening of distal ileum proximal to the ileocolic anastomosis, without frank extravasation identified. Colonoscopy revealed erythematous mucosa and multiple non-bleeding ulcers with overlying exudates around ileocolonic anastomosis and more proximally into the ileum, in addition to small caliber non-bleeding diverticula and internal hemorrhoids. Biopsies showed marked active inflammation with heavy lymphoblastic infiltrated, with eosinophils, neutrophils, as well as cryptic distortion and surface erosion. Diagnosis of capecitabine-induced ileocolitis performed based on the history and endoscopic findings. Withdrawal of capecitabine in addition to supportive care was performed, and symptoms eventually improved after a prolonged hospital course.
Discussion: While few have described that persistent diarrhea and ileitis or ileocolitis are potential complications of capecitabine use, there is even more paucity of data regarding capecitabine-associated GI bleeding. The precise mechanism of capecitabine-induced GI injury is unknown; however it has been suggested that induces loss of epithelial surface secondary to acute mucosal injury through interference with crypt cell mitoses. Our case identifies a rare but critical presentation of capecitabine-associated GI toxicity, as the treatment with capecitabine should be considered more often as a cause of severe gastrointestinal bleeding.
Disclosures:
Sandra Gomez-Paz indicated no relevant financial relationships.
Kevin Yeroushalmi indicated no relevant financial relationships.
Jiten Desai indicated no relevant financial relationships.
Deepthi Kagolanu indicated no relevant financial relationships.
Kaleem Rizvon indicated no relevant financial relationships.
Nausheer Khan indicated no relevant financial relationships.
Paul Mustacchia indicated no relevant financial relationships.
Sandra Gomez-Paz, MD, Kevin Yeroushalmi, MD, Jiten Desai, MD, Deepthi Kagolanu, MD, Kaleem Rizvon, , Nausheer Khan, MD, Paul Mustacchia, MD, MBA. B0340 - A Case of Capecitabine-Induced Gastrointestinal Hemorrhage, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
