Back

Poster Session B - Monday Morning
Category: Stomach
B0682 - Identification of Trends in Post COVID-19 Infection Gastroenterology Clinic Referrals
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Ammu Susheela, MD
Loyola Medicine, Loyola University Health System
Chicago, IL
Presenting Author(s)
Mona Lalehzari, MD1, Yalda Dehghan, MD1, Ammu Thampi Susheela, MD2, Stephen B. Hanauer, MD3
1Northwestern University Feinberg School of Medicine, Chicago, IL; 2Loyola Medicine, Loyola University Health System, Chicago, IL; 3Northwestern University, Chicago, IL
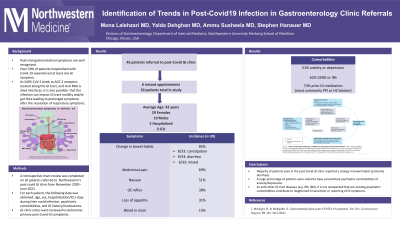
Introduction: Post-viral gastrointestinal symptoms are well recognized. Over 50% of patients hospitalized with COVID-19 experienced at least one GI symptom. Here we aim to look at longer-lasting sequelae of COVID infections on the digestive system by identifying trends in patients after the resolution of acute COVID symptoms.
Methods: A retrospective chart review was performed on all patients referred to the Northwestern Medicine post-COVID GI clinic from November 2020 - June 2021. For each patient, data regarding demographics and hospitalization/ICU stays during their COVID infection, psychiatric comorbidities, and GI history/medications were reviewed. EMR was reviewed to determine if they had changes in bowel habits, loss of appetite, nausea, GE reflux, abdominal pain, and/or bloody stools.
Results: 45 patients were referred to the clinic during this 8 month period; however, 6 missed their appointments and thus a total of 39 patients were evaluated. There were 10 males and 29 females (avg age 42). Five of these patients were hospitalized during their covid infection (three were in the ICU). The most common reported symptoms were change in bowel habits (85%), abdominal pain (69%), nausea (51%), GE reflux (38%), loss of appetite (31%), and/or bloody stools (15%). Of the 85% of patients who endorsed change in bowel habits, 8/33 reported constipation, 19/33 reported diarrhea, and 6/33 had a mixed picture. 51% of patients had a psychiatric comorbidity of anxiety or depression. 62% of patients had a prior GI history, of which GERD and IBS were the most common. 74% of patients were noted to be on a prior GI medication, of which a PPI or H2 blocker were most common.
Discussion: The majority of patients seen in the post-COVID GI clinic reported a change in bowel habits (primarily diarrhea). A large percentage of patients were also noted to have concomitant psychiatric comorbidities of depression and/or anxiety. As with other GI tract diseases (e.g. IBS, IBD), it is not unexpected that pre-existing psychiatric comorbidities contribute to a heightened GI sensitivity or reporting of GI symptoms. As SARS-CoV-2 binds to ACE-2 receptors located along the GI tract, and viral RNA is shed into feces, it is also possible that the infection can impact GI tract motility and/or gut flora leading to prolonged symptoms after the resolution of respiratory symptoms. Future longitudinal studies are anticipated to determine whether the impacts on GI function are transient or long-lasting.
Disclosures:
Mona Lalehzari, MD1, Yalda Dehghan, MD1, Ammu Thampi Susheela, MD2, Stephen B. Hanauer, MD3. B0682 - Identification of Trends in Post COVID-19 Infection Gastroenterology Clinic Referrals, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Northwestern University Feinberg School of Medicine, Chicago, IL; 2Loyola Medicine, Loyola University Health System, Chicago, IL; 3Northwestern University, Chicago, IL
Introduction: Post-viral gastrointestinal symptoms are well recognized. Over 50% of patients hospitalized with COVID-19 experienced at least one GI symptom. Here we aim to look at longer-lasting sequelae of COVID infections on the digestive system by identifying trends in patients after the resolution of acute COVID symptoms.
Methods: A retrospective chart review was performed on all patients referred to the Northwestern Medicine post-COVID GI clinic from November 2020 - June 2021. For each patient, data regarding demographics and hospitalization/ICU stays during their COVID infection, psychiatric comorbidities, and GI history/medications were reviewed. EMR was reviewed to determine if they had changes in bowel habits, loss of appetite, nausea, GE reflux, abdominal pain, and/or bloody stools.
Results: 45 patients were referred to the clinic during this 8 month period; however, 6 missed their appointments and thus a total of 39 patients were evaluated. There were 10 males and 29 females (avg age 42). Five of these patients were hospitalized during their covid infection (three were in the ICU). The most common reported symptoms were change in bowel habits (85%), abdominal pain (69%), nausea (51%), GE reflux (38%), loss of appetite (31%), and/or bloody stools (15%). Of the 85% of patients who endorsed change in bowel habits, 8/33 reported constipation, 19/33 reported diarrhea, and 6/33 had a mixed picture. 51% of patients had a psychiatric comorbidity of anxiety or depression. 62% of patients had a prior GI history, of which GERD and IBS were the most common. 74% of patients were noted to be on a prior GI medication, of which a PPI or H2 blocker were most common.
Discussion: The majority of patients seen in the post-COVID GI clinic reported a change in bowel habits (primarily diarrhea). A large percentage of patients were also noted to have concomitant psychiatric comorbidities of depression and/or anxiety. As with other GI tract diseases (e.g. IBS, IBD), it is not unexpected that pre-existing psychiatric comorbidities contribute to a heightened GI sensitivity or reporting of GI symptoms. As SARS-CoV-2 binds to ACE-2 receptors located along the GI tract, and viral RNA is shed into feces, it is also possible that the infection can impact GI tract motility and/or gut flora leading to prolonged symptoms after the resolution of respiratory symptoms. Future longitudinal studies are anticipated to determine whether the impacts on GI function are transient or long-lasting.
Disclosures:
Mona Lalehzari indicated no relevant financial relationships.
Yalda Dehghan indicated no relevant financial relationships.
Ammu Thampi Susheela indicated no relevant financial relationships.
Stephen Hanauer: Abbvie – Advisor or Review Panel Member, Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau. allergan – Consultant, Grant/Research Support. Amgen – Consultant, Grant/Research Support. Arena – Advisor or Review Panel Member, Advisory Committee/Board Member. BMS – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau. Boehringer-Ingelheim – Advisor or Review Panel Member, Advisory Committee/Board Member. gilead – Consultant, Grant/Research Support. gossamer – Advisor or Review Panel Member. gsk – Consultant, Grant/Research Support. Janssen – Advisor or Review Panel Member, Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau. lilly – Grant/Research Support. Merck – Consultant. Novartis – Consultant. Pfizer – Advisor or Review Panel Member, Advisory Committee/Board Member, Speakers Bureau. prometheus – Advisory Committee/Board Member, Consultant, Grant/Research Support. Protagonist – Advisor or Review Panel Member, Advisory Committee/Board Member. seres – Consultant. seres therapeutics – Consultant. Takeda – Advisor or Review Panel Member, Advisory Committee/Board Member, Consultant, Speakers Bureau.
Mona Lalehzari, MD1, Yalda Dehghan, MD1, Ammu Thampi Susheela, MD2, Stephen B. Hanauer, MD3. B0682 - Identification of Trends in Post COVID-19 Infection Gastroenterology Clinic Referrals, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
