Back

Poster Session B - Monday Morning
Category: Colon
B0158 - A Case of Post-SARS-CoV-2 Colitis
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Azubuogu Anudu, MD
University of South Florida
Tampa, FL
Presenting Author(s)
Azubuogu Anudu, MD, Liza Plafsky, MD, Jonathan Hilal, MD
University of South Florida, Tampa, FL
Introduction: We present a case of colitis following SARS-CoV-2 (SCV2) infection in a patient with simultaneous liver-kidney transplantation (SLK). SCV2 is primarily a respiratory illness, with unique consequences being identified on a regular basis. We believe that given the temporal relationship between SCV2 diagnosis and endoscopic findings, the viral infection played a role in our patient’s disease pathogenesis.
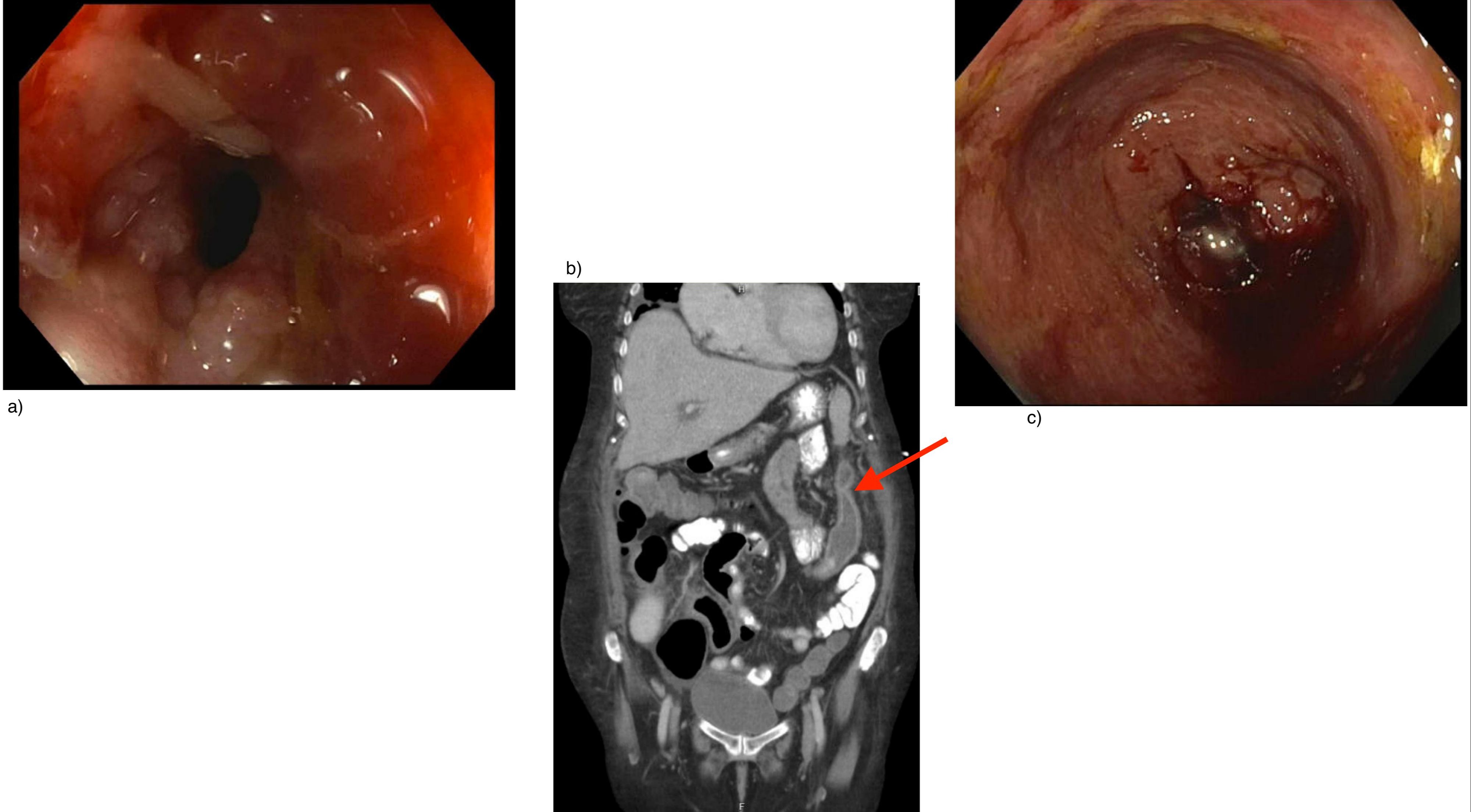
Case Description/Methods: A 67-year-old white woman with a history of end-stage liver disease, complicated by hepatorenal syndrome, underwent a SLK. Following SLK, the patient's hospital course was complicated by SCV2 infection, 57 days after admission. The GI service was consulted prior to SCV2 infection for melena and performed an EGD which was non-diagnostic. GI was re-consulted 3.5 weeks after her SCV2 diagnosis due to worsening anemia, prompting a colonoscopy (CLN) that showed an obstructive stricture at the splenic flexure that could not be traversed. Colonic biopsies were non-diagnostic, showing granulation tissue, hemorrhage, and edema but no dysplasia or chronic inflammation. Infectious stool studies were negative, and biopsies were negative for CMV and HSV. CT abdomen/pelvis (A/P) performed immediately after CLN showed a colonic stricture (CS) at the splenic flexure in addition to terminal ileum/colonic inflammation, possibly secondary to fibrostenotic Crohn’s disease. Of note, the patient had a normal CLN in 2017 and CT A/P done one day prior to SCV2 infection was unremarkable.
Given the inconclusive diagnosis and implications of adding more immunosuppressants to the patient's existing post-transplant treatment regimen, a repeat CLN was performed to establish a firm diagnosis. This CLN was performed 9 days after the first and re-demonstrated a fibrostenotic CS at the splenic flexure with balloon dilation being performed to allow scope passage. The terminal ileum and entire colon had diffuse circumferential inflammation with erythema, friability, and shallow ulcerations. Biopsies showed architectural distortion and ulceration with markedly inflamed granulation tissue but once again, no chronic inflammation. With all other causes of acute colitis having been ruled out, the patient was diagnosed with post-SCV2 colitis.
Discussion: Our case demonstrates one of the less commonly seen gastrointestinal complications of this novel viral pathogen, and we believe that it will broaden the horizons of physicians with regards to the possible sequelae of SCV2 infection.
Disclosures:
Azubuogu Anudu, MD, Liza Plafsky, MD, Jonathan Hilal, MD. B0158 - A Case of Post-SARS-CoV-2 Colitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
University of South Florida, Tampa, FL
Introduction: We present a case of colitis following SARS-CoV-2 (SCV2) infection in a patient with simultaneous liver-kidney transplantation (SLK). SCV2 is primarily a respiratory illness, with unique consequences being identified on a regular basis. We believe that given the temporal relationship between SCV2 diagnosis and endoscopic findings, the viral infection played a role in our patient’s disease pathogenesis.
Case Description/Methods: A 67-year-old white woman with a history of end-stage liver disease, complicated by hepatorenal syndrome, underwent a SLK. Following SLK, the patient's hospital course was complicated by SCV2 infection, 57 days after admission. The GI service was consulted prior to SCV2 infection for melena and performed an EGD which was non-diagnostic. GI was re-consulted 3.5 weeks after her SCV2 diagnosis due to worsening anemia, prompting a colonoscopy (CLN) that showed an obstructive stricture at the splenic flexure that could not be traversed. Colonic biopsies were non-diagnostic, showing granulation tissue, hemorrhage, and edema but no dysplasia or chronic inflammation. Infectious stool studies were negative, and biopsies were negative for CMV and HSV. CT abdomen/pelvis (A/P) performed immediately after CLN showed a colonic stricture (CS) at the splenic flexure in addition to terminal ileum/colonic inflammation, possibly secondary to fibrostenotic Crohn’s disease. Of note, the patient had a normal CLN in 2017 and CT A/P done one day prior to SCV2 infection was unremarkable.
Given the inconclusive diagnosis and implications of adding more immunosuppressants to the patient's existing post-transplant treatment regimen, a repeat CLN was performed to establish a firm diagnosis. This CLN was performed 9 days after the first and re-demonstrated a fibrostenotic CS at the splenic flexure with balloon dilation being performed to allow scope passage. The terminal ileum and entire colon had diffuse circumferential inflammation with erythema, friability, and shallow ulcerations. Biopsies showed architectural distortion and ulceration with markedly inflamed granulation tissue but once again, no chronic inflammation. With all other causes of acute colitis having been ruled out, the patient was diagnosed with post-SCV2 colitis.
Discussion: Our case demonstrates one of the less commonly seen gastrointestinal complications of this novel viral pathogen, and we believe that it will broaden the horizons of physicians with regards to the possible sequelae of SCV2 infection.
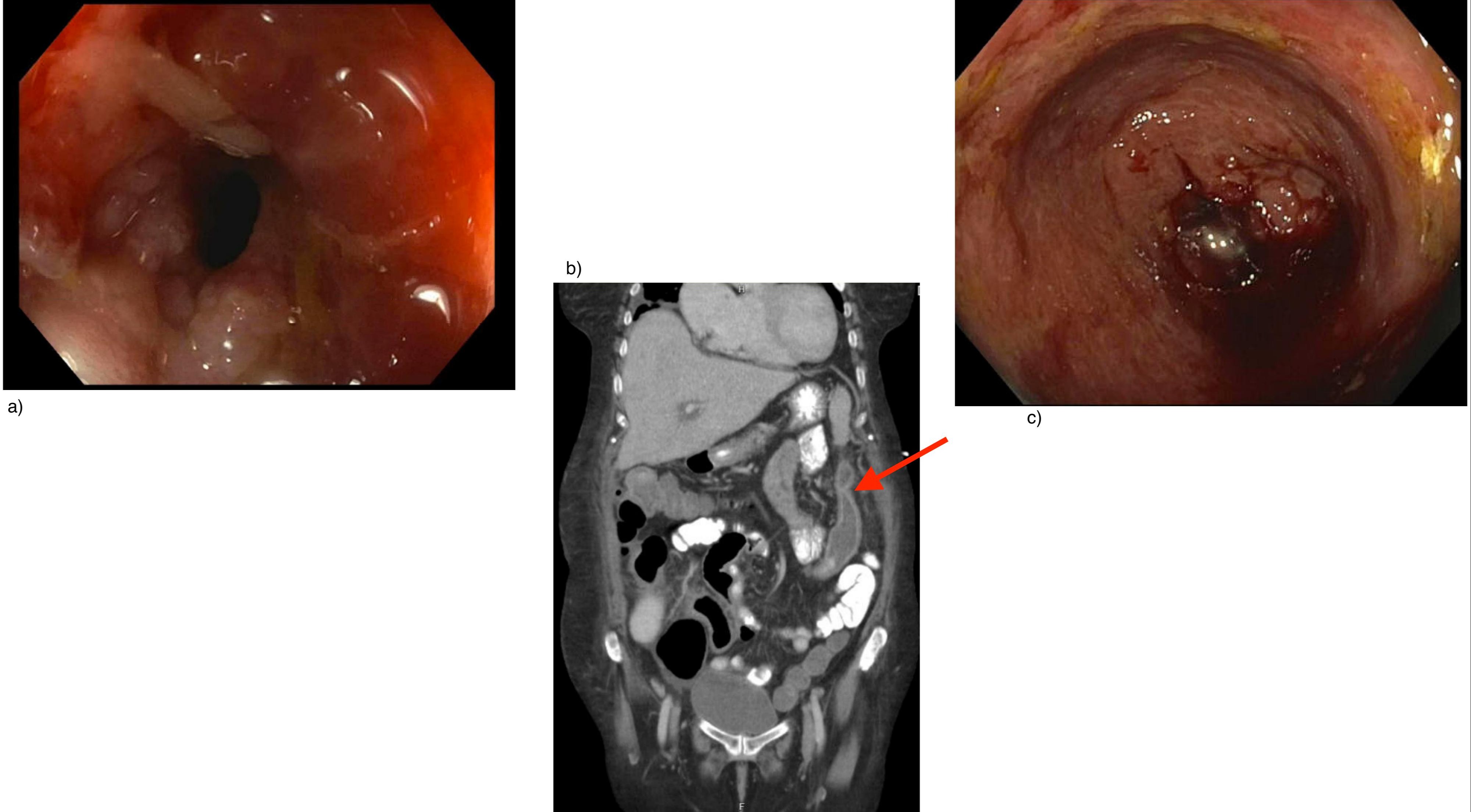
Figure: Figure 1. a) Colonoscopy showing stricture/colitis present at the level of the splenic flexure. b) Coronal CT-abdomen/pelvis with IV and PO contrast showing a segment of focal narrowing at the splenic flexure which could represent stricture (Red arrow). c) Colonoscopy showing colitis present in the ascending colon.
Disclosures:
Azubuogu Anudu indicated no relevant financial relationships.
Liza Plafsky indicated no relevant financial relationships.
Jonathan Hilal indicated no relevant financial relationships.
Azubuogu Anudu, MD, Liza Plafsky, MD, Jonathan Hilal, MD. B0158 - A Case of Post-SARS-CoV-2 Colitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

