Back

Poster Session C - Monday Afternoon
Category: Esophagus
C0249 - A Rare Cause of Dysphagia: Esophageal Stricture Due to Lichen Planus
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio
.jpg)
Ayushi Shah, MBBS
Houston Methodist Hospital
Houston, TX
Presenting Author(s)
Ayushi Shah, MBBS, Michelle Jones-Pauley, DO, Mary R. Schwartz, MD, Neha Mathur, MD
Houston Methodist Hospital, Houston, TX
Introduction: Esophageal lichen planus (ELP) is an unusual and under-recognized cause of dysphagia. Timely diagnosis is crucial for effective treatment as ELP has been associated with increased risk for development of squamous cell carcinoma.
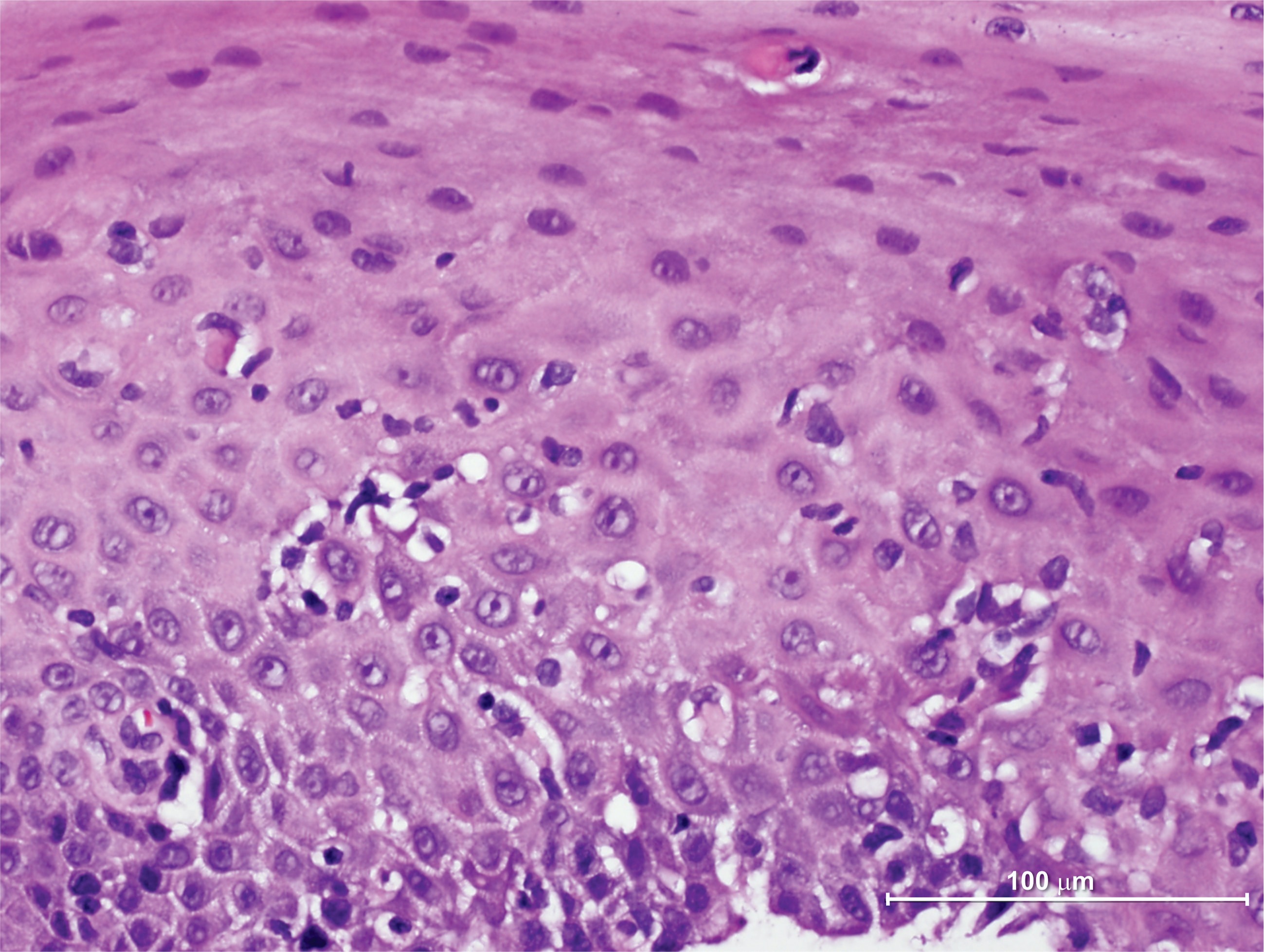
Case Description/Methods: A 72-year-old man presented with esophageal dysphagia to solids. Past medical history included oral lichen planus (LP) and osteoporosis with use of alendronate. He underwent endoscopy (EGD) which showed a proximal esophageal stricture for which balloon dilation ranging from 8 to 15 mm was done. Biopsy of the stricture showed esophageal mucosa with increased intraepithelial eosinophils. The working diagnosis was peptic stricture with possible eosinophilic esophagitis(EoE). He was started on pantoprazole 40 mg twice daily. He underwent two more EGDs with dilation for recurrent stricture and on the 2nd EGD, biopsy of the stricture showed numerous intraepithelial lymphocytes and focal apoptotic squamous cells (Civatte bodies) compatible with ELP. Budesonide slurry 1 mg twice daily was instituted and an EGD 6 months later showed near-resolution of the stricture. The patient no longer requires dilations or antiacid therapy and is asymptomatic currently. He had Candida esophagitis 1 month after initiation of budesonide which was treated with fluconazole.
Discussion: ELP is prevalent in patients with mucocutaneous forms of LP, most often oral LP. It is rarely seen in males with a case series by Franco et al describing the female to male ratio as 5:1. The endoscopic differential diagnosis for ELP should distinguish findings of esophagitis and stricture secondary to EoE, reflux esophagitis or esophageal Candidiasis. A low threshold should be kept for suspecting ELP in a patient with dysphagia and mucocutaneous LP. If histology is inconclusive but a high index of suspicion remains, particularly in patients with mucosal LP, repeating biopsies may be warranted for diagnosis as is highlighted in this case. A co-relation between longer duration of disease with severity of inflammation has been proposed with case series reporting strictures. Treatment includes serial dilations, topical and/or systemic steroids. Recurrence has been described despite topical steroid therapy with requirement of additional dilations. Successful use of immunomodulators such as cyclosporine, mycophenolate has been described. There is paucity of data regarding surveillance and optimal treatment for ELP, and thus further studies are needed for better understanding of this disease.
Disclosures:
Ayushi Shah, MBBS, Michelle Jones-Pauley, DO, Mary R. Schwartz, MD, Neha Mathur, MD. C0249 - A Rare Cause of Dysphagia: Esophageal Stricture Due to Lichen Planus, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Houston Methodist Hospital, Houston, TX
Introduction: Esophageal lichen planus (ELP) is an unusual and under-recognized cause of dysphagia. Timely diagnosis is crucial for effective treatment as ELP has been associated with increased risk for development of squamous cell carcinoma.
Case Description/Methods: A 72-year-old man presented with esophageal dysphagia to solids. Past medical history included oral lichen planus (LP) and osteoporosis with use of alendronate. He underwent endoscopy (EGD) which showed a proximal esophageal stricture for which balloon dilation ranging from 8 to 15 mm was done. Biopsy of the stricture showed esophageal mucosa with increased intraepithelial eosinophils. The working diagnosis was peptic stricture with possible eosinophilic esophagitis(EoE). He was started on pantoprazole 40 mg twice daily. He underwent two more EGDs with dilation for recurrent stricture and on the 2nd EGD, biopsy of the stricture showed numerous intraepithelial lymphocytes and focal apoptotic squamous cells (Civatte bodies) compatible with ELP. Budesonide slurry 1 mg twice daily was instituted and an EGD 6 months later showed near-resolution of the stricture. The patient no longer requires dilations or antiacid therapy and is asymptomatic currently. He had Candida esophagitis 1 month after initiation of budesonide which was treated with fluconazole.
Discussion: ELP is prevalent in patients with mucocutaneous forms of LP, most often oral LP. It is rarely seen in males with a case series by Franco et al describing the female to male ratio as 5:1. The endoscopic differential diagnosis for ELP should distinguish findings of esophagitis and stricture secondary to EoE, reflux esophagitis or esophageal Candidiasis. A low threshold should be kept for suspecting ELP in a patient with dysphagia and mucocutaneous LP. If histology is inconclusive but a high index of suspicion remains, particularly in patients with mucosal LP, repeating biopsies may be warranted for diagnosis as is highlighted in this case. A co-relation between longer duration of disease with severity of inflammation has been proposed with case series reporting strictures. Treatment includes serial dilations, topical and/or systemic steroids. Recurrence has been described despite topical steroid therapy with requirement of additional dilations. Successful use of immunomodulators such as cyclosporine, mycophenolate has been described. There is paucity of data regarding surveillance and optimal treatment for ELP, and thus further studies are needed for better understanding of this disease.
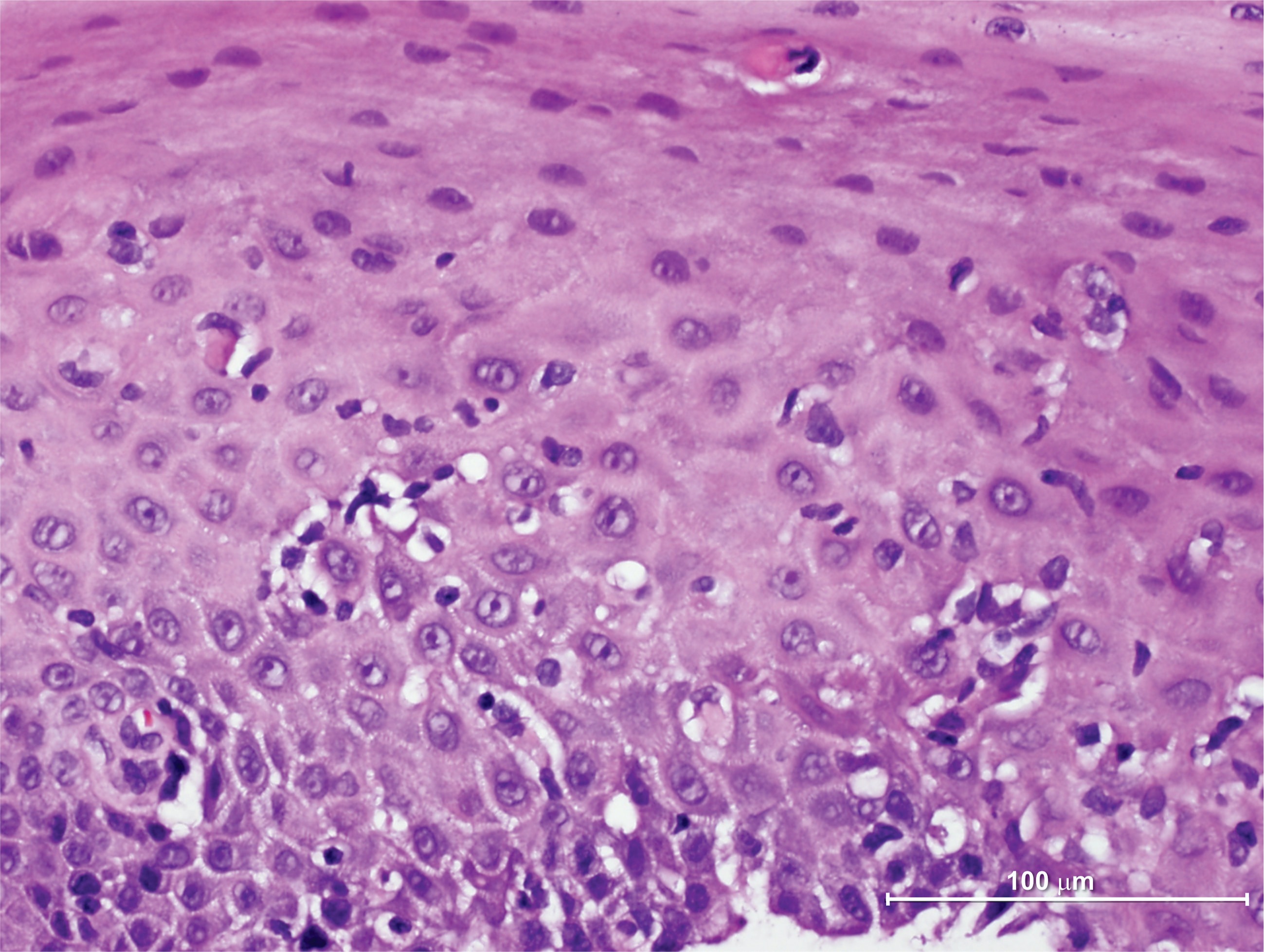
Figure: Esophageal biopsy showing esophageal squamous mucosa with basal cell hyperplasia, intraepithelial lymphocytes, and two apoptotic keratinocytes (Civatte or colloid bodies). Findings are compatible with esophageal lichen planus.
Disclosures:
Ayushi Shah indicated no relevant financial relationships.
Michelle Jones-Pauley indicated no relevant financial relationships.
Mary Schwartz indicated no relevant financial relationships.
Neha Mathur indicated no relevant financial relationships.
Ayushi Shah, MBBS, Michelle Jones-Pauley, DO, Mary R. Schwartz, MD, Neha Mathur, MD. C0249 - A Rare Cause of Dysphagia: Esophageal Stricture Due to Lichen Planus, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
