Back

Poster Session C - Monday Afternoon
Category: Esophagus
C0258 - Pseudoachalasia due to Metastatic Prostate Adenocarcinoma
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Anthony P. Nguyen, MD
University of New Mexico
Albuquerque, New Mexico
Presenting Author(s)
Anthony P. Nguyen, MD1, Fray Arroyo, MD1, Marjan Hovaida, MD2
1University of New Mexico, Albuquerque, NM; 2University of California, Davis, Sacramento, CA
Introduction: Pseudoachalasia (also known as “secondary achalasia”) is a condition in which esophageal dysmotility and impaired relaxation of the lower esophageal sphincter (LES) occur due to a secondary etiology such as tumor invasion or a paraneoplastic syndrome. The literature shows that only 4% of all cases of achalasia are diagnosed as pseudoachalasia and of those cases, up to 70% are due to esophageal adenocarcinoma. The early distinction between primary and secondary achalasia is important for patient outcomes as their treatments differ greatly and delayed diagnosis can cause progression of an underlying malignancy. This is especially important in cases in which the underlying malignancy is related to metastases from a distant site as the presentation of disease can be atypical.
Case Description/Methods: Here we describe a case of a 76 year-old man presenting with unintentional weight loss and new onset dysphagia to solids and eventually liquids. Esophagogastroduodenoscopy (EGD) was notable for a hypertonic LES with mild resistance to scope passage. CT abdomen & pelvis showed a 2.4cm x 1.5cm mediastinal mass with enlarged mediastinal lymph nodes. Barium swallow showed no intraluminal defect while manometry results were consistent with type II achalasia per Chicago Classification. Endoscopic ultrasound with biopsy revealed metastatic prostate adenocarcinoma and patient was referred to Oncology clinic for further treatment.
Discussion: This patient presented with classic symptoms of achalasia with dysphagia and weight loss and after thorough diagnostic evaluation was found to have pseudoachalasia due to mass effect from an underlying malignancy. Although esophageal adenocarcinoma is the culprit malignancy 70% of the time, this patient was diagnosed with distant metastases from prostate adenocarcinoma prior to having any urologic symptoms. Timely differentiation of achalasia from pseudoachalasia presents a diagnostic challenge as the two conditions are often clinically homogenous. This case presents an opportunity to highlight the clinical and endoscopic findings more often found in pseudoachalasia compared to achalasia. When compared to primary achalasia, pseudoachalasia is associated with a much shorter duration of symptoms, a greater severity of weight loss lower integration relaxation pressure on esophageal manometry and inducible relaxation of the LES with amyl nitrate. Knowledge of these relatively more predictive signs can lead to a faster diagnosis and ultimately better patient outcomes.

Disclosures:
Anthony P. Nguyen, MD1, Fray Arroyo, MD1, Marjan Hovaida, MD2. C0258 - Pseudoachalasia due to Metastatic Prostate Adenocarcinoma, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of New Mexico, Albuquerque, NM; 2University of California, Davis, Sacramento, CA
Introduction: Pseudoachalasia (also known as “secondary achalasia”) is a condition in which esophageal dysmotility and impaired relaxation of the lower esophageal sphincter (LES) occur due to a secondary etiology such as tumor invasion or a paraneoplastic syndrome. The literature shows that only 4% of all cases of achalasia are diagnosed as pseudoachalasia and of those cases, up to 70% are due to esophageal adenocarcinoma. The early distinction between primary and secondary achalasia is important for patient outcomes as their treatments differ greatly and delayed diagnosis can cause progression of an underlying malignancy. This is especially important in cases in which the underlying malignancy is related to metastases from a distant site as the presentation of disease can be atypical.
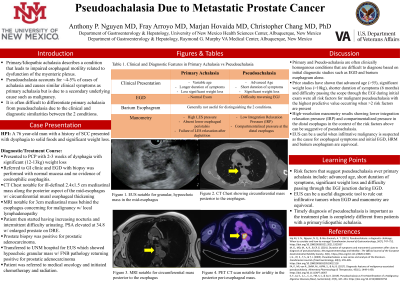
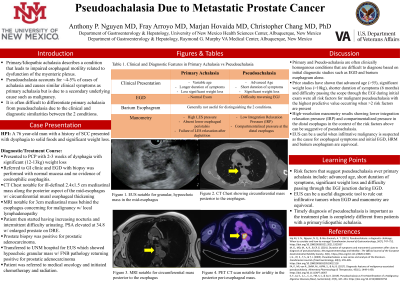
Case Description/Methods: Here we describe a case of a 76 year-old man presenting with unintentional weight loss and new onset dysphagia to solids and eventually liquids. Esophagogastroduodenoscopy (EGD) was notable for a hypertonic LES with mild resistance to scope passage. CT abdomen & pelvis showed a 2.4cm x 1.5cm mediastinal mass with enlarged mediastinal lymph nodes. Barium swallow showed no intraluminal defect while manometry results were consistent with type II achalasia per Chicago Classification. Endoscopic ultrasound with biopsy revealed metastatic prostate adenocarcinoma and patient was referred to Oncology clinic for further treatment.
Discussion: This patient presented with classic symptoms of achalasia with dysphagia and weight loss and after thorough diagnostic evaluation was found to have pseudoachalasia due to mass effect from an underlying malignancy. Although esophageal adenocarcinoma is the culprit malignancy 70% of the time, this patient was diagnosed with distant metastases from prostate adenocarcinoma prior to having any urologic symptoms. Timely differentiation of achalasia from pseudoachalasia presents a diagnostic challenge as the two conditions are often clinically homogenous. This case presents an opportunity to highlight the clinical and endoscopic findings more often found in pseudoachalasia compared to achalasia. When compared to primary achalasia, pseudoachalasia is associated with a much shorter duration of symptoms, a greater severity of weight loss lower integration relaxation pressure on esophageal manometry and inducible relaxation of the LES with amyl nitrate. Knowledge of these relatively more predictive signs can lead to a faster diagnosis and ultimately better patient outcomes.

Figure: Hypoechogenic mass seen on endoscopic ultrasonography (EUS) in the middle mediastinum.
Disclosures:
Anthony Nguyen indicated no relevant financial relationships.
Fray Arroyo indicated no relevant financial relationships.
Marjan Hovaida indicated no relevant financial relationships.
Anthony P. Nguyen, MD1, Fray Arroyo, MD1, Marjan Hovaida, MD2. C0258 - Pseudoachalasia due to Metastatic Prostate Adenocarcinoma, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
