Back


Poster Session C - Monday Afternoon
Category: Esophagus
C0265 - Acute Esophageal Necrosis Due to Posterior Inferior Cerebellar Artery Stroke
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Has Audio

Brittany M. Woods, DO
AdventHealth Redmond
Rome, GA
Presenting Author(s)
Brittany M. Woods, DO1, Mary Abkemeier, MD2, Zubda Talat, MD1, Louis E. Lataif, MD3
1AdventHealth Redmond, Rome, GA; 2Ascension Saint Francis Hospital, Evanston, IL; 3Rome Gastroenterology Associates, Rome, GA
Introduction: Strokes involving the cerebellum can cause severe vomiting and lead to significant morbidity. Intractable vomiting after cerebellar stroke may be a precursor for the development of acute esophageal necrosis (AEN). Acute esophageal necrosis is a rare syndrome in which presumed hypoperfusion predisposes the esophagus to severe injury via reflux of acid and pepsin. It can be seen in association with protracted vomiting. In this case, we report the development of AEN related to vomiting from posterior inferior cerebellar artery (PICA) stroke.
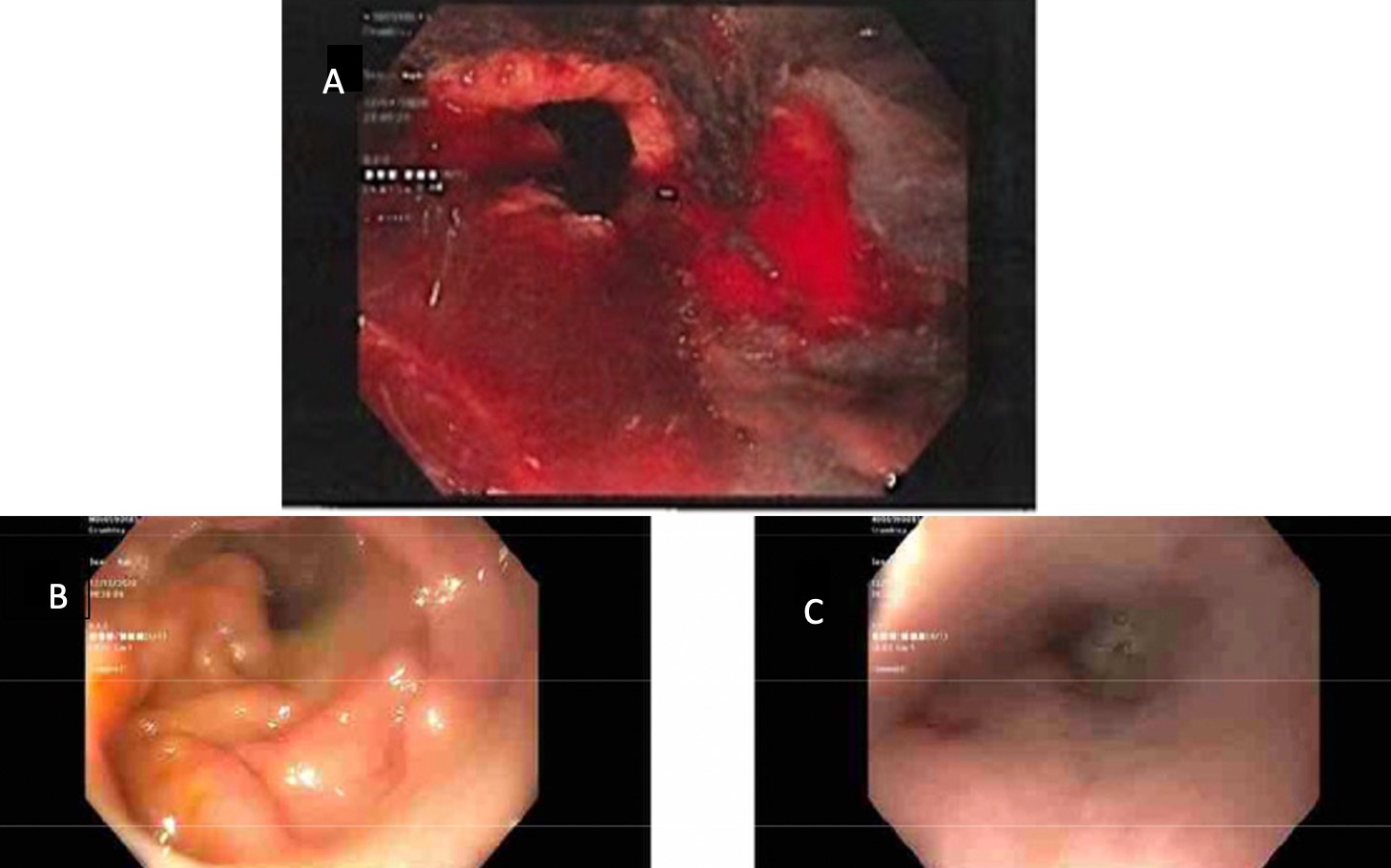
Case Description/Methods: A 59-year-old male with past medical history of diabetes, hypertension, and GERD presented with intractable vomiting and dizziness for one week. Imaging revealed a subacute stroke of the right inferior cerebellum in the distribution of the right PICA. His nausea and vomiting were initially difficult to control with first line antiemetics, but after 4 days oral intake and nausea improved enough for safe discharge home with plans to continue vestibular therapy. Two days later, he returned to the hospital with more severe vomiting, dizziness, and dehydration. Multiple anti-emetics were tried unsuccessfully. Despite these efforts at symptom control, he continued to have retching and nausea. On hospital day 2, he developed brisk hematemesis requiring emergent upper endoscopy. He was found to have severe esophagitis with an area of circumferential necrosis in the distal esophagus, consistent with AEN (photo A). Bleeding was treated with hemoclips (Resolution Clips, Boston Scientific) and epinephrine. In order to avoid further emesis and esophageal necrosis, the patient was left under deep sedation with intubation and was monitored in the ICU. The following day, a J tube was placed surgically. On day 6, surveillance EGD revealed complete resolution of necrosis with only white exudate remaining (photo B,C). After improvement in mental status, the patient was extubated on hospital day 12 and returned to baseline mentation. Oral feedings were reintroduced after extubation. The patient fully recovered.
Discussion: This case demonstrates a previously undescribed presentation of acute esophageal necrosis as a complication of an acute right PICA infarct associated with intractable vomiting. Our approach using prolonged deep sedation, intubation, and jejunal feelings avoided further retching and allowed healing of necrotic esophageal mucosa. This case report may serve as a model for care of this rare syndrome and may stimulate further study.
Disclosures:
Brittany M. Woods, DO1, Mary Abkemeier, MD2, Zubda Talat, MD1, Louis E. Lataif, MD3. C0265 - Acute Esophageal Necrosis Due to Posterior Inferior Cerebellar Artery Stroke, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1AdventHealth Redmond, Rome, GA; 2Ascension Saint Francis Hospital, Evanston, IL; 3Rome Gastroenterology Associates, Rome, GA
Introduction: Strokes involving the cerebellum can cause severe vomiting and lead to significant morbidity. Intractable vomiting after cerebellar stroke may be a precursor for the development of acute esophageal necrosis (AEN). Acute esophageal necrosis is a rare syndrome in which presumed hypoperfusion predisposes the esophagus to severe injury via reflux of acid and pepsin. It can be seen in association with protracted vomiting. In this case, we report the development of AEN related to vomiting from posterior inferior cerebellar artery (PICA) stroke.
Case Description/Methods: A 59-year-old male with past medical history of diabetes, hypertension, and GERD presented with intractable vomiting and dizziness for one week. Imaging revealed a subacute stroke of the right inferior cerebellum in the distribution of the right PICA. His nausea and vomiting were initially difficult to control with first line antiemetics, but after 4 days oral intake and nausea improved enough for safe discharge home with plans to continue vestibular therapy. Two days later, he returned to the hospital with more severe vomiting, dizziness, and dehydration. Multiple anti-emetics were tried unsuccessfully. Despite these efforts at symptom control, he continued to have retching and nausea. On hospital day 2, he developed brisk hematemesis requiring emergent upper endoscopy. He was found to have severe esophagitis with an area of circumferential necrosis in the distal esophagus, consistent with AEN (photo A). Bleeding was treated with hemoclips (Resolution Clips, Boston Scientific) and epinephrine. In order to avoid further emesis and esophageal necrosis, the patient was left under deep sedation with intubation and was monitored in the ICU. The following day, a J tube was placed surgically. On day 6, surveillance EGD revealed complete resolution of necrosis with only white exudate remaining (photo B,C). After improvement in mental status, the patient was extubated on hospital day 12 and returned to baseline mentation. Oral feedings were reintroduced after extubation. The patient fully recovered.
Discussion: This case demonstrates a previously undescribed presentation of acute esophageal necrosis as a complication of an acute right PICA infarct associated with intractable vomiting. Our approach using prolonged deep sedation, intubation, and jejunal feelings avoided further retching and allowed healing of necrotic esophageal mucosa. This case report may serve as a model for care of this rare syndrome and may stimulate further study.
Figure: Figure A shows evidence of acute esophageal necrosis of the distal esophagus. Photo B and C show endoscopic findings of white exudate and recovery of prior necrotic esophagus.
Disclosures:
Brittany Woods indicated no relevant financial relationships.
Mary Abkemeier indicated no relevant financial relationships.
Zubda Talat indicated no relevant financial relationships.
Louis Lataif indicated no relevant financial relationships.
Brittany M. Woods, DO1, Mary Abkemeier, MD2, Zubda Talat, MD1, Louis E. Lataif, MD3. C0265 - Acute Esophageal Necrosis Due to Posterior Inferior Cerebellar Artery Stroke, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
