Back


Poster Session C - Monday Afternoon
Category: GI Bleeding
C0314 - Impact of Non-Alcoholic Fatty Liver Disease on In-Patient Outcomes in Non-Variceal Upper Gastrointestinal Bleeding: A Nationwide Analysis
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Has Audio

Aakriti Soni, MD
Saint Vincent Hospital
Worcester, MA
Presenting Author(s)
Aakriti Soni, MD1, Anuroop Yekula, MD1, Nitish Sood, 2, Kannu Bansal, MD1, Aaron Douen, MD3, George M. Abraham, MD, MPH1
1Saint Vincent Hospital, Worcester, MA; 2Medical College of Georgia, Augusta, GA; 3Coney Island Hospital, Brooklyn, NY
Introduction: Non-Alcoholic Fatty Liver Disease (NAFLD) is the leading cause of liver disease globally with an estimated prevalence of 25%. The clinical and economic burden of NAFLD is expected to keep increasing. Upper gastrointestinal bleeding (UGIB) occurs in ~100 out of 100,000 people per year. Our aim with this study is to determine the impact of NAFLD on mortality, in-patient complications, and utilization of resources in patients with UGIB.
Methods: Using de-identified data from the National Inpatient Sample (NIS) database 2016-2019, we identified patients with non-variceal UGIB and then stratified them into those with and without NAFLD. Patient demographics, length of stay, hospital charges, comorbidities, complications and mortality outcome data were analyzed. Mann-Whitney tests with Bonferroni corrections were used for testing differences in continuous variables, while chi-squared tests with Bonferroni corrections were used for testing homogeneity of categorical variables. Multivariate logistic regression was conducted to analyze the relationship between mortality and NAFLD, while controlling for relevant covariates. Bidirectional stepwise regression was utilized to build the final model. All statistical analysis and hypothesis tests were performed at significance level, with p-value set at < 0.05. Analyses were conducted using R software (v. 4.0.4).
Results: Multivariate logistic regression analysis (MLRA) was conducted, controlling for the multiple covariates.The primary outcome of interest, mortality, was found to be significantly higher in patients with NAFLD and GI bleeding [aOR: 1.88 (1.68-2.1)]. Secondary outcomes of interest, shock [aOR: 1.15 (1.07-1.22)], acute respiratory failure [aOR:1.28 (1.15-1.42)] and acute liver failure [aOR:5.58 (4.48-6.69)] were all more likely to occur in this cohort. Patients with NAFLD were also more likely to incur higher hospital charges [$2174 ($1677-$2618)] and have a longer length of stay [0.28 days (0.17-0.38)]. Interestingly, in our study the patients with NAFLD were less likely to suffer from acute myocardial infarction [aOR: 0.73 (0.64-0.85)]. Patients with NAFLD were not more likely to suffer AKI, shock requiring vasopressors, sepsis, blood transfusion, intubation or dialysis.
Discussion: Our analysis showed that patients with non-variceal UGIB have higher mortality, increased complications, longer length of stay and higher hospital charges pointing to the increased morbidity and economic burden of NAFLD.
Disclosures:
Aakriti Soni, MD1, Anuroop Yekula, MD1, Nitish Sood, 2, Kannu Bansal, MD1, Aaron Douen, MD3, George M. Abraham, MD, MPH1. C0314 - Impact of Non-Alcoholic Fatty Liver Disease on In-Patient Outcomes in Non-Variceal Upper Gastrointestinal Bleeding: A Nationwide Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Saint Vincent Hospital, Worcester, MA; 2Medical College of Georgia, Augusta, GA; 3Coney Island Hospital, Brooklyn, NY
Introduction: Non-Alcoholic Fatty Liver Disease (NAFLD) is the leading cause of liver disease globally with an estimated prevalence of 25%. The clinical and economic burden of NAFLD is expected to keep increasing. Upper gastrointestinal bleeding (UGIB) occurs in ~100 out of 100,000 people per year. Our aim with this study is to determine the impact of NAFLD on mortality, in-patient complications, and utilization of resources in patients with UGIB.
Methods: Using de-identified data from the National Inpatient Sample (NIS) database 2016-2019, we identified patients with non-variceal UGIB and then stratified them into those with and without NAFLD. Patient demographics, length of stay, hospital charges, comorbidities, complications and mortality outcome data were analyzed. Mann-Whitney tests with Bonferroni corrections were used for testing differences in continuous variables, while chi-squared tests with Bonferroni corrections were used for testing homogeneity of categorical variables. Multivariate logistic regression was conducted to analyze the relationship between mortality and NAFLD, while controlling for relevant covariates. Bidirectional stepwise regression was utilized to build the final model. All statistical analysis and hypothesis tests were performed at significance level, with p-value set at < 0.05. Analyses were conducted using R software (v. 4.0.4).
Results: Multivariate logistic regression analysis (MLRA) was conducted, controlling for the multiple covariates.The primary outcome of interest, mortality, was found to be significantly higher in patients with NAFLD and GI bleeding [aOR: 1.88 (1.68-2.1)]. Secondary outcomes of interest, shock [aOR: 1.15 (1.07-1.22)], acute respiratory failure [aOR:1.28 (1.15-1.42)] and acute liver failure [aOR:5.58 (4.48-6.69)] were all more likely to occur in this cohort. Patients with NAFLD were also more likely to incur higher hospital charges [$2174 ($1677-$2618)] and have a longer length of stay [0.28 days (0.17-0.38)]. Interestingly, in our study the patients with NAFLD were less likely to suffer from acute myocardial infarction [aOR: 0.73 (0.64-0.85)]. Patients with NAFLD were not more likely to suffer AKI, shock requiring vasopressors, sepsis, blood transfusion, intubation or dialysis.
Discussion: Our analysis showed that patients with non-variceal UGIB have higher mortality, increased complications, longer length of stay and higher hospital charges pointing to the increased morbidity and economic burden of NAFLD.
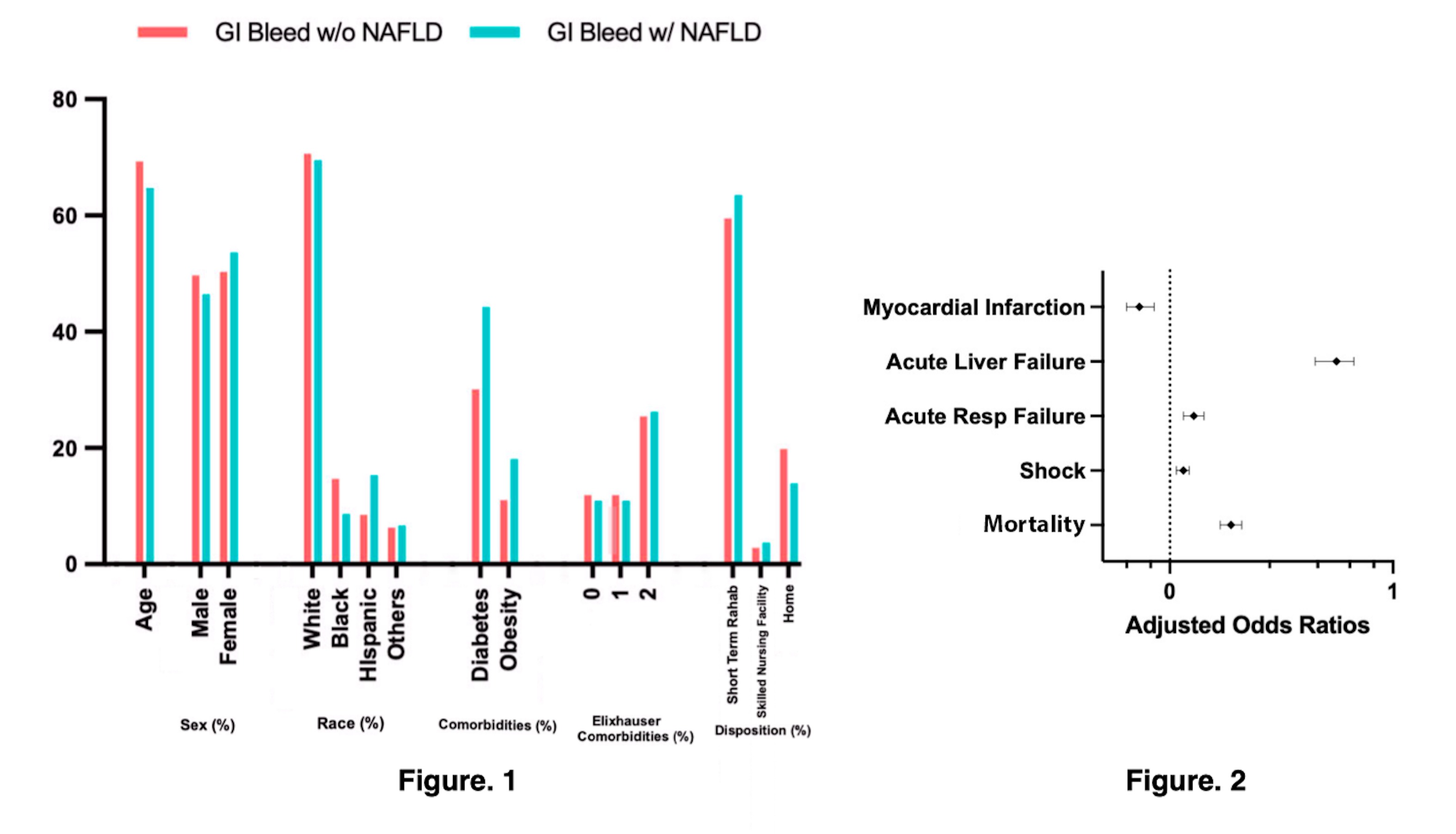
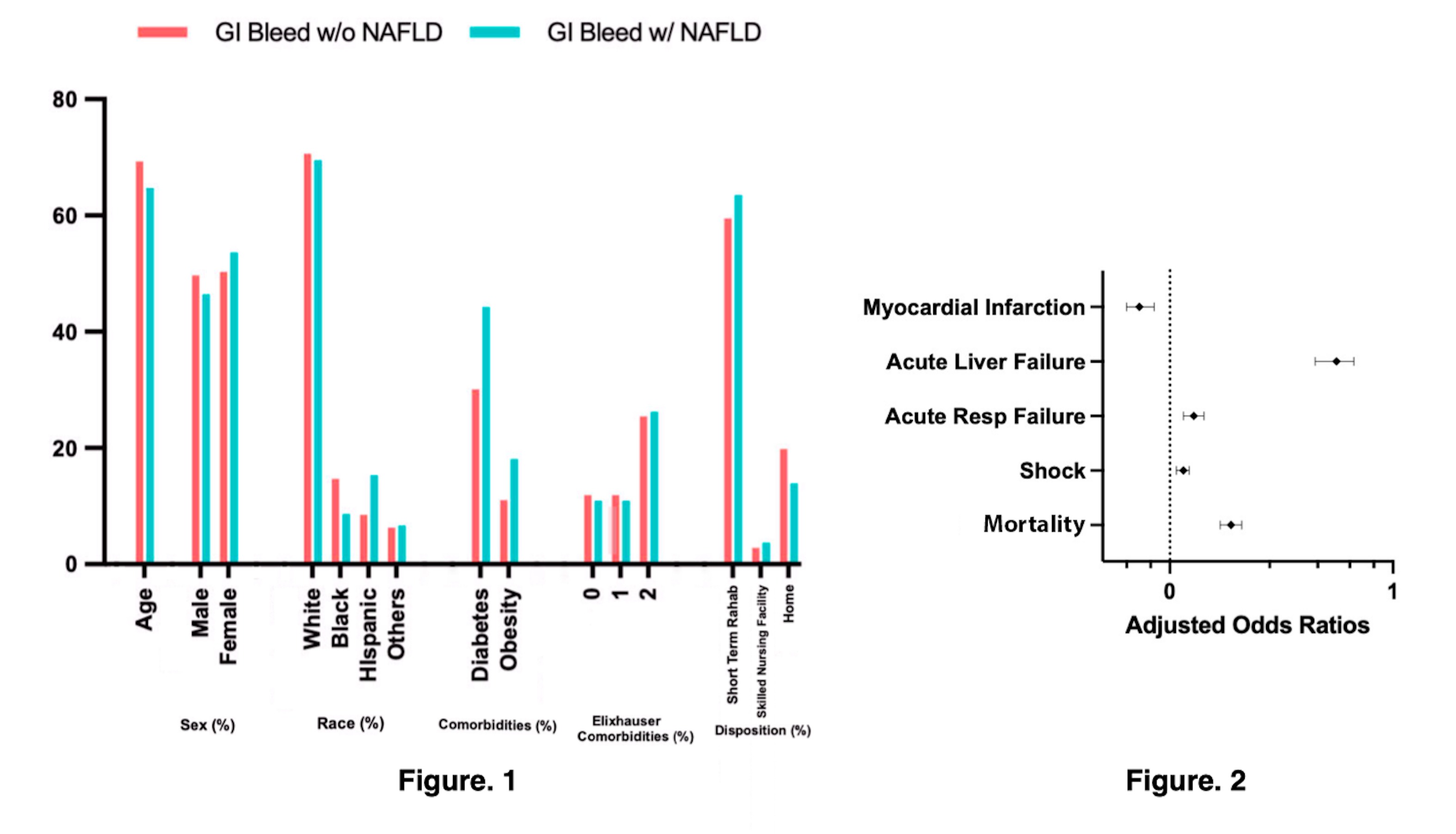
Figure: Figure 1: Comparison of demographic and co-morbidities data between non-variceal UGIB with and without NAFLD.
Figure 2: Forest Plot showing relation between presence of NAFLD with GI bleeding and co-variates.
Figure 2: Forest Plot showing relation between presence of NAFLD with GI bleeding and co-variates.
Disclosures:
Aakriti Soni indicated no relevant financial relationships.
Anuroop Yekula indicated no relevant financial relationships.
Nitish Sood indicated no relevant financial relationships.
Kannu Bansal indicated no relevant financial relationships.
Aaron Douen indicated no relevant financial relationships.
George Abraham indicated no relevant financial relationships.
Aakriti Soni, MD1, Anuroop Yekula, MD1, Nitish Sood, 2, Kannu Bansal, MD1, Aaron Douen, MD3, George M. Abraham, MD, MPH1. C0314 - Impact of Non-Alcoholic Fatty Liver Disease on In-Patient Outcomes in Non-Variceal Upper Gastrointestinal Bleeding: A Nationwide Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

