Back

Poster Session C - Monday Afternoon
Category: GI Bleeding
C0315 - Increased Mortality and Length of Stay in Patients With Gastrointestinal Bleeding With Cardiovascular Disease Compared to Patients Without Cardiovascular Disease
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Usha Thapa, MD
Trihealth Good Samaritan Hospital
Cincinnati, OH
Presenting Author(s)
Usha Thapa, MD1, Cynthia Contreras, MD2, Joe Alfeghaly, MD3, Leonid Khokhlov, MD3, Sarthak Aryal, MD1
1Trihealth Good Samaritan Hospital, Cincinnati, OH; 2Trihealth, Cincinnati, OH; 3TriHealth, Cincinnati, OH
Introduction: Patients with cardiovascular diseases are commonly treated with antiplatelet or anticoagulation therapy which increases the risk of gastrointestinal bleeding. We compared morbidities, in-hospital mortality rates, and LOS in patients hospitalized for gastrointestinal bleeding with known cardiovascular disease to those without cardiovascular disease
Methods: This retrospective cohort study was conducted using Electronic Medical Records from 2013 to 2020. Patients admitted with gastrointestinal bleeding with established cardiovascular disease (1470) were compared to the patients without cardiovascular disease (4717). Baseline demographic data and outcomes were compared using Mann-Whitney U test, Chi square test and logistic regression. A p-value of < 0.05 was considered significant.
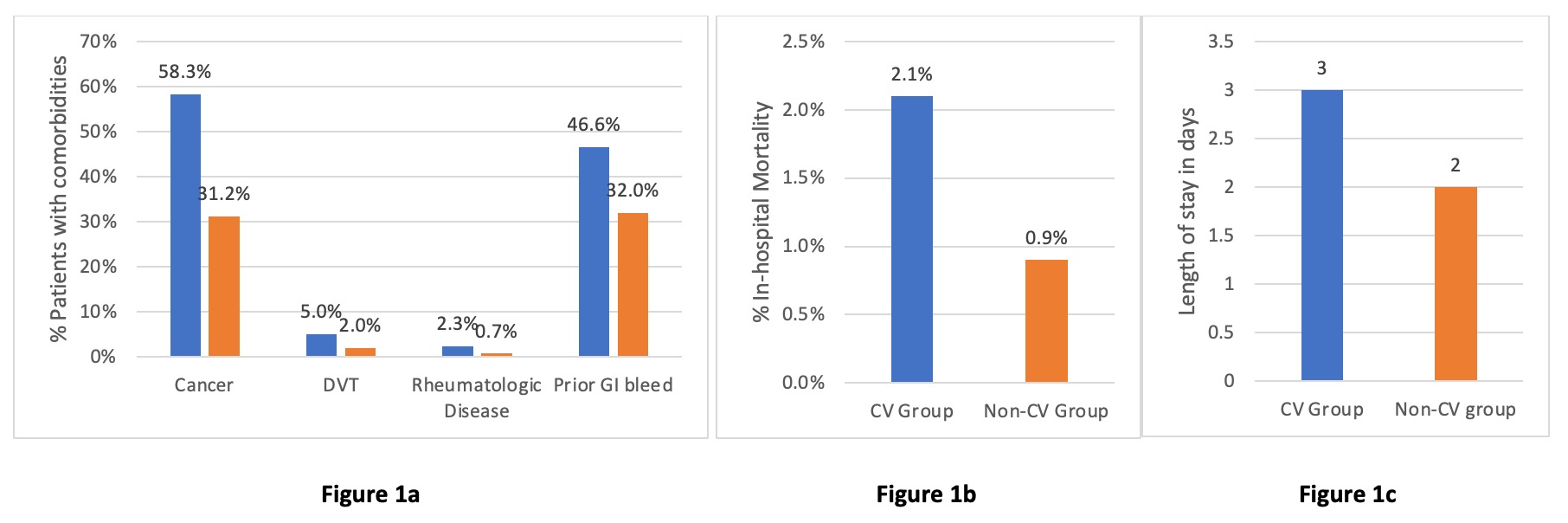
Results: Among 6187 patients admitted with gastrointestinal bleeding, 23% (1470) had cardiovascular disease and 77% (4717) did not have cardiovascular disease. Patients with gastrointestinal bleeding with cardiovascular comorbidities were older, 78 [69-85] vs. 68 [55-80], and had more male population, 51.4% (755) vs 47.9% (2258). Patients with gastrointestinal bleeding with cardiovascular disease had increased prevalence of cancer (58.3% vs. 31.2%), prior gastrointestinal bleeding (46% vs. 32%), DVT (5% vs. 2%), & rheumatologic disease (2.3% vs. 0.7%). Patients with gastrointestinal bleeding with cardiovascular disease had significantly higher BNP (375 vs. 157, p< 0.001), CRP (38 vs. 15, p=0.008), & ESR (47 vs. 27, p=0.004). Higher prevalence of aspirin use (24.1% vs. 16.2%, p< 0.001), DAPT use (1% vs. 0.4%, p=0.006), & anticoagulation (20.1% vs. 2.9%, p< 0.001) was seen in patients with gastrointestinal bleed with cardiovascular disease. LOS (3 vs. 2 days, p< 0.001) & in-hospital mortality (2.1% vs. 0.9% p< 0.001) during hospitalization were significantly higher in patients with GI bleed with cardiovascular disease.
Discussion: Patients with gastrointestinal bleeding who had cardiovascular disease have a higher prevalence of chronic comorbidities and increased use of antiplatelet and anticoagulation therapy. There was longer length of stay and increased in-hospital mortality in this group during hospitalization. Higher prevalence of cancer among patients with gastrointestinal bleeding with cardiovascular disease may also be linked to poor outcomes. Further investigation is required to assess these outcomes and define patients' characteristics.
Disclosures:
Usha Thapa, MD1, Cynthia Contreras, MD2, Joe Alfeghaly, MD3, Leonid Khokhlov, MD3, Sarthak Aryal, MD1. C0315 - Increased Mortality and Length of Stay in Patients With Gastrointestinal Bleeding With Cardiovascular Disease Compared to Patients Without Cardiovascular Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Trihealth Good Samaritan Hospital, Cincinnati, OH; 2Trihealth, Cincinnati, OH; 3TriHealth, Cincinnati, OH
Introduction: Patients with cardiovascular diseases are commonly treated with antiplatelet or anticoagulation therapy which increases the risk of gastrointestinal bleeding. We compared morbidities, in-hospital mortality rates, and LOS in patients hospitalized for gastrointestinal bleeding with known cardiovascular disease to those without cardiovascular disease
Methods: This retrospective cohort study was conducted using Electronic Medical Records from 2013 to 2020. Patients admitted with gastrointestinal bleeding with established cardiovascular disease (1470) were compared to the patients without cardiovascular disease (4717). Baseline demographic data and outcomes were compared using Mann-Whitney U test, Chi square test and logistic regression. A p-value of < 0.05 was considered significant.
Results: Among 6187 patients admitted with gastrointestinal bleeding, 23% (1470) had cardiovascular disease and 77% (4717) did not have cardiovascular disease. Patients with gastrointestinal bleeding with cardiovascular comorbidities were older, 78 [69-85] vs. 68 [55-80], and had more male population, 51.4% (755) vs 47.9% (2258). Patients with gastrointestinal bleeding with cardiovascular disease had increased prevalence of cancer (58.3% vs. 31.2%), prior gastrointestinal bleeding (46% vs. 32%), DVT (5% vs. 2%), & rheumatologic disease (2.3% vs. 0.7%). Patients with gastrointestinal bleeding with cardiovascular disease had significantly higher BNP (375 vs. 157, p< 0.001), CRP (38 vs. 15, p=0.008), & ESR (47 vs. 27, p=0.004). Higher prevalence of aspirin use (24.1% vs. 16.2%, p< 0.001), DAPT use (1% vs. 0.4%, p=0.006), & anticoagulation (20.1% vs. 2.9%, p< 0.001) was seen in patients with gastrointestinal bleed with cardiovascular disease. LOS (3 vs. 2 days, p< 0.001) & in-hospital mortality (2.1% vs. 0.9% p< 0.001) during hospitalization were significantly higher in patients with GI bleed with cardiovascular disease.
Discussion: Patients with gastrointestinal bleeding who had cardiovascular disease have a higher prevalence of chronic comorbidities and increased use of antiplatelet and anticoagulation therapy. There was longer length of stay and increased in-hospital mortality in this group during hospitalization. Higher prevalence of cancer among patients with gastrointestinal bleeding with cardiovascular disease may also be linked to poor outcomes. Further investigation is required to assess these outcomes and define patients' characteristics.
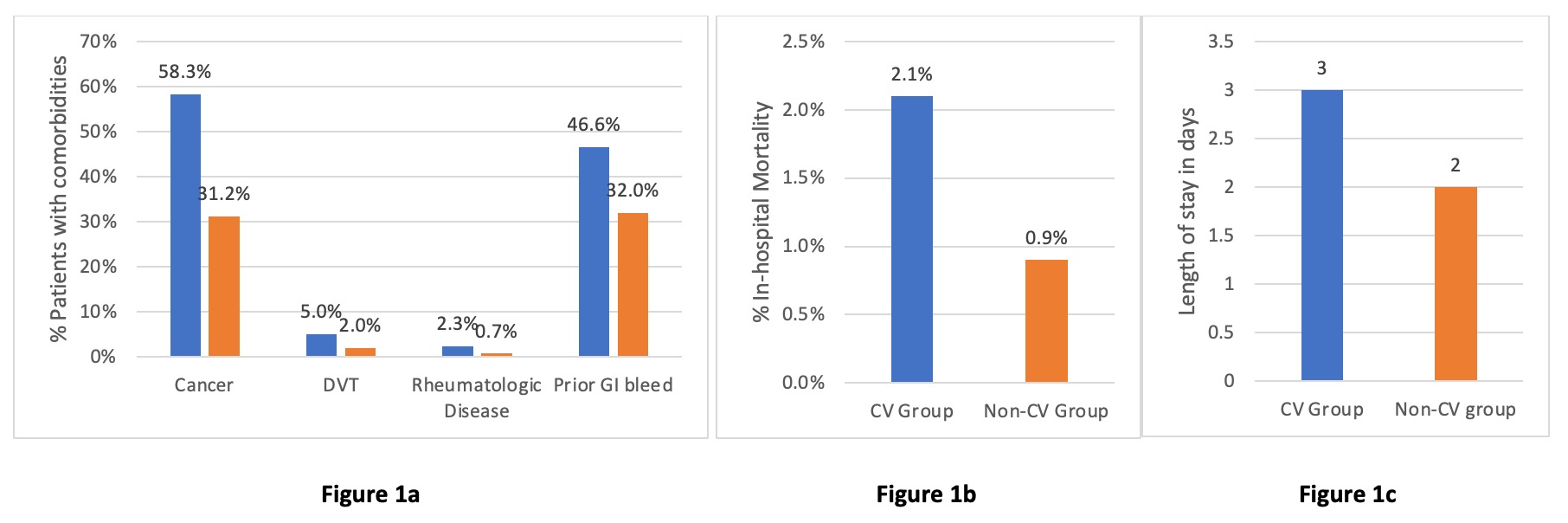
Figure: Figure 1a: Prevalence of other comorbidities including cancer, rheumatological diseases, DVT and prior gastrointestinal bleeding in patients admitted with gastrointestinal bleeding stratified by patients with and without cardiovascular disease. Cardiovascular disease cohort represented by blue bar and non-cardiovascular cohort represented by orange bar, p-value <0.001
Figure 1b. In-hospital mortality rates in patients admitted with gastrointestinal bleeding stratified by patients with and without cardiovascular diseases. p-value < 0.001
Figure 1c. Median length of stay in days in patients admitted with gastrointestinal bleeding stratified by patients with and without cardiovascular diseases. p-value <0.001
Figure 1b. In-hospital mortality rates in patients admitted with gastrointestinal bleeding stratified by patients with and without cardiovascular diseases. p-value < 0.001
Figure 1c. Median length of stay in days in patients admitted with gastrointestinal bleeding stratified by patients with and without cardiovascular diseases. p-value <0.001
Disclosures:
Usha Thapa indicated no relevant financial relationships.
Cynthia Contreras indicated no relevant financial relationships.
Joe Alfeghaly indicated no relevant financial relationships.
Leonid Khokhlov indicated no relevant financial relationships.
Sarthak Aryal indicated no relevant financial relationships.
Usha Thapa, MD1, Cynthia Contreras, MD2, Joe Alfeghaly, MD3, Leonid Khokhlov, MD3, Sarthak Aryal, MD1. C0315 - Increased Mortality and Length of Stay in Patients With Gastrointestinal Bleeding With Cardiovascular Disease Compared to Patients Without Cardiovascular Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
