Back

Poster Session C - Monday Afternoon
Category: GI Bleeding
C0332 - Gastrointestinal Hemorrhage From Hepaticojejunal Varices: A Rare Complication of Pancreaticoduodenectomy
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Peter Block, MD
Yale School of Medicine
New Haven, Connecticut
Presenting Author(s)
Peter Block, MD1, Anish C. Gonchigar, MD2, James J. Farrell, MD3, Darrick K. Li, MD, PhD3
1Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA; 2Yale New Haven Hospital, New Haven, CT; 3Yale University School of Medicine, New Haven, CT
Introduction: Ectopic varices are portosystemic collaterals that form outside the esophageal-gastric region and frequently pose a diagnostic and therapeutic challenge. Rarely, bleeding from ectopic varices can occur as a complication of pancreatic surgery. We describe a case of gastrointestinal bleeding from ectopic hepaticojejunal varices after pancreaticoduodenectomy.
Case Description/Methods: A 66-year-old man with a history of intraductal papillary mucinous neoplasm (PMN) with high-grade dysplasia status post Whipple procedure two years previously, presented to the hospital with melena. His Whipple procedure had been complicated by splenic vein thrombosis and disease recurrence, necessitating further debridement three months prior to presentation. On examination, his vital signs were stable and there were no stigmata of liver disease. His laboratory tests were notable for a hemoglobin 8.0 g/dL (from baseline of 11 g/dL), platelets 174 x 109/L, BUN 29 mg/dL, INR 1.0.
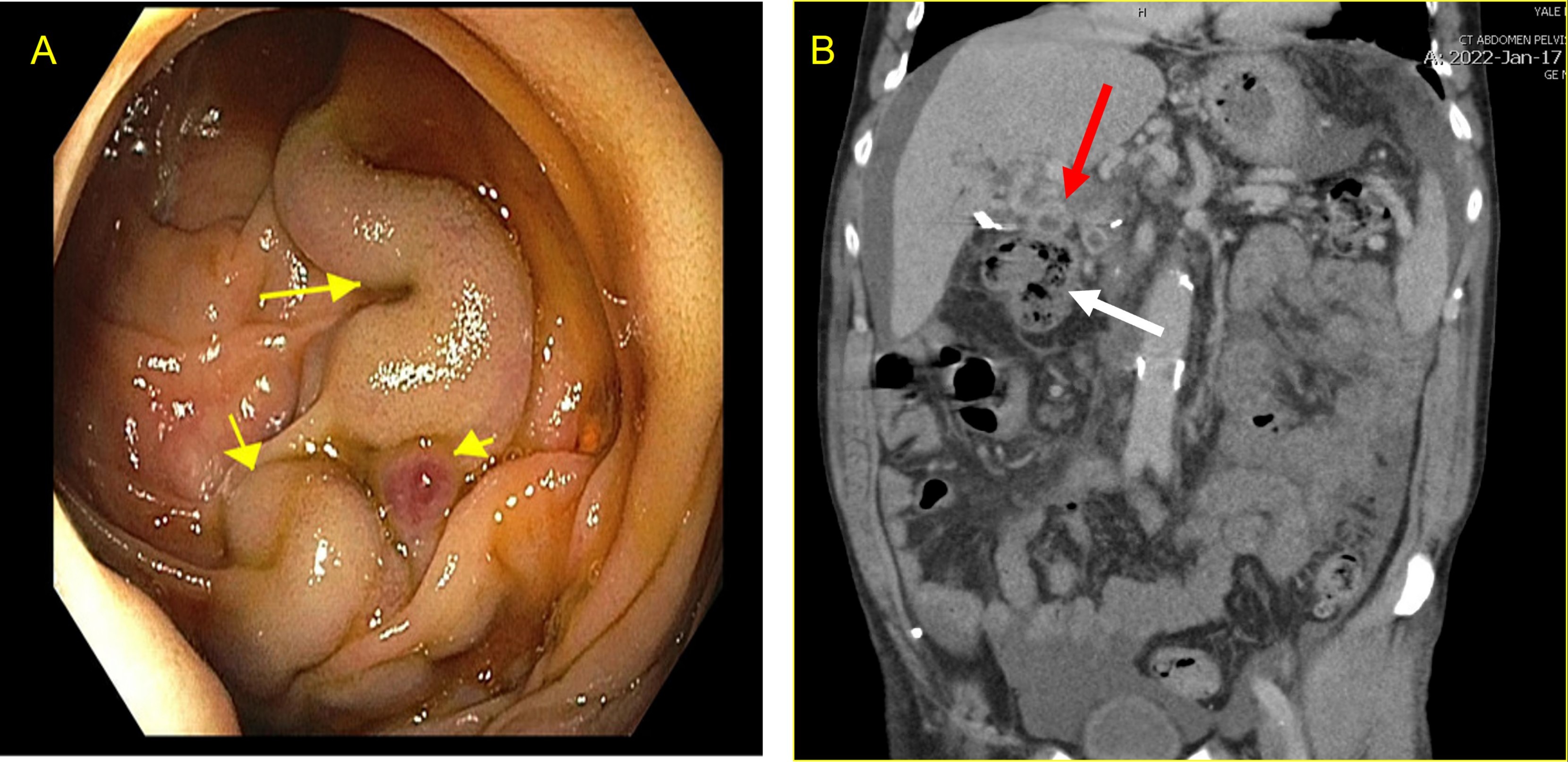
He initially underwent EGD and colonoscopy, which were unremarkable. A second look endoscopy was performed and deep intubation of the afferent limb revealed ectopic varices with stigmata of recent bleeding at the hepaticojejunostomy (Panel A). Cross-sectional imaging demonstrated a patent splenic vein but chronic occlusion of the portal and proximal superior mesenteric veins with cavernous transformation, extensive upper abdominal varices and splenomegaly (Panel B). There was no clinical or radiologic evidence of cirrhosis. After multidisciplinary discussion, an endovascular approach was deemed technically infeasible given extensive chronic mesenteric thrombus and a surgical approach was deemed prohibitively high-risk. The patient ultimately underwent endoscopic injection of 2-octyl cyanoacrylate into the ectopic varices and has remained without recurrent bleeding in over 5 months of follow-up.
Discussion: Hemorrhage from ectopic jejunal varices following pancreatic surgery has previously been described in only a few case reports. Given the potential for vascular injury and local inflammation, these procedures can result in mesenteric venous thrombosis with subsequent ectopic variceal formation. If present, defining the vascular supply of varices with early multi-disciplinary involvement is paramount to their management. Multiple treatments have been reported, including portal venous stenting, embolization, and local sclerotherapy or cyanoacrylate injection as in this case.
Disclosures:
Peter Block, MD1, Anish C. Gonchigar, MD2, James J. Farrell, MD3, Darrick K. Li, MD, PhD3. C0332 - Gastrointestinal Hemorrhage From Hepaticojejunal Varices: A Rare Complication of Pancreaticoduodenectomy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA; 2Yale New Haven Hospital, New Haven, CT; 3Yale University School of Medicine, New Haven, CT
Introduction: Ectopic varices are portosystemic collaterals that form outside the esophageal-gastric region and frequently pose a diagnostic and therapeutic challenge. Rarely, bleeding from ectopic varices can occur as a complication of pancreatic surgery. We describe a case of gastrointestinal bleeding from ectopic hepaticojejunal varices after pancreaticoduodenectomy.
Case Description/Methods: A 66-year-old man with a history of intraductal papillary mucinous neoplasm (PMN) with high-grade dysplasia status post Whipple procedure two years previously, presented to the hospital with melena. His Whipple procedure had been complicated by splenic vein thrombosis and disease recurrence, necessitating further debridement three months prior to presentation. On examination, his vital signs were stable and there were no stigmata of liver disease. His laboratory tests were notable for a hemoglobin 8.0 g/dL (from baseline of 11 g/dL), platelets 174 x 109/L, BUN 29 mg/dL, INR 1.0.
He initially underwent EGD and colonoscopy, which were unremarkable. A second look endoscopy was performed and deep intubation of the afferent limb revealed ectopic varices with stigmata of recent bleeding at the hepaticojejunostomy (Panel A). Cross-sectional imaging demonstrated a patent splenic vein but chronic occlusion of the portal and proximal superior mesenteric veins with cavernous transformation, extensive upper abdominal varices and splenomegaly (Panel B). There was no clinical or radiologic evidence of cirrhosis. After multidisciplinary discussion, an endovascular approach was deemed technically infeasible given extensive chronic mesenteric thrombus and a surgical approach was deemed prohibitively high-risk. The patient ultimately underwent endoscopic injection of 2-octyl cyanoacrylate into the ectopic varices and has remained without recurrent bleeding in over 5 months of follow-up.
Discussion: Hemorrhage from ectopic jejunal varices following pancreatic surgery has previously been described in only a few case reports. Given the potential for vascular injury and local inflammation, these procedures can result in mesenteric venous thrombosis with subsequent ectopic variceal formation. If present, defining the vascular supply of varices with early multi-disciplinary involvement is paramount to their management. Multiple treatments have been reported, including portal venous stenting, embolization, and local sclerotherapy or cyanoacrylate injection as in this case.
Figure: (A) Ectopic varices (yellow arrows) are noted in the afferent limb at the hepaticojejunostomy. (B) Coronal view of computed tomography scan of abdomen demonstrating large upper abdominal collaterals (red arrow) that drain close to the afferent limb (white arrow).
Disclosures:
Peter Block indicated no relevant financial relationships.
Anish Gonchigar indicated no relevant financial relationships.
James Farrell indicated no relevant financial relationships.
Darrick Li indicated no relevant financial relationships.
Peter Block, MD1, Anish C. Gonchigar, MD2, James J. Farrell, MD3, Darrick K. Li, MD, PhD3. C0332 - Gastrointestinal Hemorrhage From Hepaticojejunal Varices: A Rare Complication of Pancreaticoduodenectomy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

