Back

Poster Session C - Monday Afternoon
Category: Colon
C0142 - Colonic Merkel Cell Carcinoma of Unknown Primary: Small Cell Carcinoma Outside the Usual
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Brandon Ganjineh
Virginia Tech Carilion School of Medicine
Roanoke, VA
Presenting Author(s)
Brandon Ganjineh, , William Abel, MD, Shravani Reddy, MD, Kiley Fagan, MD, Douglas Grider, MD
Virginia Tech Carilion School of Medicine, Roanoke, VA
Introduction: Merkel cell carcinoma (MCC) is a rare neuroendocrine skin carcinoma with documented metastases to the liver, lungs, and gastrointestinal (GI) tract. Colonic metastases are rare but seen with recurrent or primary cutaneous lesions. Described is a patient who presented with bowel obstruction with a hepatic flexure MCC of unknown primary (MCCUP).
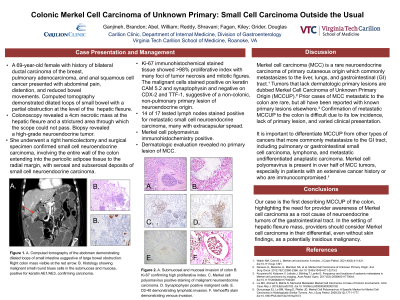
Case Description/Methods: A 69-year-old female with a history of breast, lung, and anal cancer presented to the emergency department with abdominal pain and distension. Computed tomography of her abdomen demonstrated dilated loops of small bowel and a partial obstruction with transition point in the hepatic flexure.
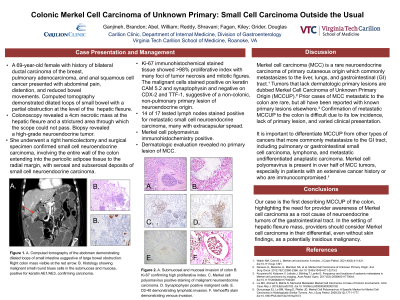
Colonoscopy demonstrated a 4 cm mass at the hepatic flexure obstructing the lumen. Biopsy revealed a high-grade neuroendocrine carcinoma. A right colectomy and histopathology confirmed small cell neuroendocrine carcinoma involving the colonic wall into the pericolic adipose tissue with nodal involvement. It was positive on cytokeratin CAM 5.2, synaptophysin, and Merkel cell polyomavirus (MCPvY) and negative on CDX-2 and TTF-1, excluding primary bowel or lung small cell carcinomas, respectively. Dermatologic evaluation did not reveal a primary cutaneous lesion. Genetic testing was unremarkable.
Discussion: This is the first case of MCCUP presenting with colonic obstruction; prior described cases of MCC metastatic to the colon were recurrent disease or from primary skin lesions. Because MCC is rare, has non-specific symptoms, and may lack a primary lesion, MCCUP must be distinguished from other small round blue cell malignancies more commonly found in the GI tract. Thus, neuroendocrine, keratin and MCPyV ancillary staining are critical to distinguish MCC from B-cell lymphoma, small cell carcinoma of bowel or lung primary, and other metastatic dermal malignancies. MCPyV testing in the absence of prior diagnosis is uncommon but vital to the workup of neuroendocrine carcinomas when CDX-2 and TTF-1 are negative as MCPyV positive lymph nodes predict worse outcomes such as disease-free survival. In this patient immunosuppression and prior radiation increased the risk of MCC, and even suggest that this might be a colonic primary.
Rarely, MCC and MCCUP are root causes of neuroendocrine carcinomas of the GI tract. In immunocompromised patients, biopsy and pathologic staining are necessary to distinguish insidious malignancies. MCPyV analysis is helpful for diagnosing MCCUP and informing its prognosis.

Disclosures:
Brandon Ganjineh, , William Abel, MD, Shravani Reddy, MD, Kiley Fagan, MD, Douglas Grider, MD. C0142 - Colonic Merkel Cell Carcinoma of Unknown Primary: Small Cell Carcinoma Outside the Usual, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Virginia Tech Carilion School of Medicine, Roanoke, VA
Introduction: Merkel cell carcinoma (MCC) is a rare neuroendocrine skin carcinoma with documented metastases to the liver, lungs, and gastrointestinal (GI) tract. Colonic metastases are rare but seen with recurrent or primary cutaneous lesions. Described is a patient who presented with bowel obstruction with a hepatic flexure MCC of unknown primary (MCCUP).
Case Description/Methods: A 69-year-old female with a history of breast, lung, and anal cancer presented to the emergency department with abdominal pain and distension. Computed tomography of her abdomen demonstrated dilated loops of small bowel and a partial obstruction with transition point in the hepatic flexure.
Colonoscopy demonstrated a 4 cm mass at the hepatic flexure obstructing the lumen. Biopsy revealed a high-grade neuroendocrine carcinoma. A right colectomy and histopathology confirmed small cell neuroendocrine carcinoma involving the colonic wall into the pericolic adipose tissue with nodal involvement. It was positive on cytokeratin CAM 5.2, synaptophysin, and Merkel cell polyomavirus (MCPvY) and negative on CDX-2 and TTF-1, excluding primary bowel or lung small cell carcinomas, respectively. Dermatologic evaluation did not reveal a primary cutaneous lesion. Genetic testing was unremarkable.
Discussion: This is the first case of MCCUP presenting with colonic obstruction; prior described cases of MCC metastatic to the colon were recurrent disease or from primary skin lesions. Because MCC is rare, has non-specific symptoms, and may lack a primary lesion, MCCUP must be distinguished from other small round blue cell malignancies more commonly found in the GI tract. Thus, neuroendocrine, keratin and MCPyV ancillary staining are critical to distinguish MCC from B-cell lymphoma, small cell carcinoma of bowel or lung primary, and other metastatic dermal malignancies. MCPyV testing in the absence of prior diagnosis is uncommon but vital to the workup of neuroendocrine carcinomas when CDX-2 and TTF-1 are negative as MCPyV positive lymph nodes predict worse outcomes such as disease-free survival. In this patient immunosuppression and prior radiation increased the risk of MCC, and even suggest that this might be a colonic primary.
Rarely, MCC and MCCUP are root causes of neuroendocrine carcinomas of the GI tract. In immunocompromised patients, biopsy and pathologic staining are necessary to distinguish insidious malignancies. MCPyV analysis is helpful for diagnosing MCCUP and informing its prognosis.
Disclosures:
Brandon Ganjineh indicated no relevant financial relationships.
William Abel indicated no relevant financial relationships.
Shravani Reddy indicated no relevant financial relationships.
Kiley Fagan indicated no relevant financial relationships.
Douglas Grider indicated no relevant financial relationships.
Brandon Ganjineh, , William Abel, MD, Shravani Reddy, MD, Kiley Fagan, MD, Douglas Grider, MD. C0142 - Colonic Merkel Cell Carcinoma of Unknown Primary: Small Cell Carcinoma Outside the Usual, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
