Back

Poster Session C - Monday Afternoon
Category: GI Bleeding
C0346 - A Case of Hemorrhagic Cholecystitis and Bleeding Duodenal (Ulcer): A Rare Coincidence!
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Busara Songtanin, MD
Texas Tech University Health Sciences Center
Lubbock, Texas
Presenting Author(s)
Busara Songtanin, MD1, Kenneth Nugent, MD1, Kanak Das, MD2
1Texas Tech University Health Sciences Center, Lubbock, TX; 2Texas Tech University Health Sciences Center and University Medical Center, Lubbock, TX
Introduction: Hemorrhagic cholecystitis is a life-threatening condition and may result in death if not treated promptly. Here, we present an atypical case of hemorrhagic cholecystitis that presented with melena but no abdominal pain.
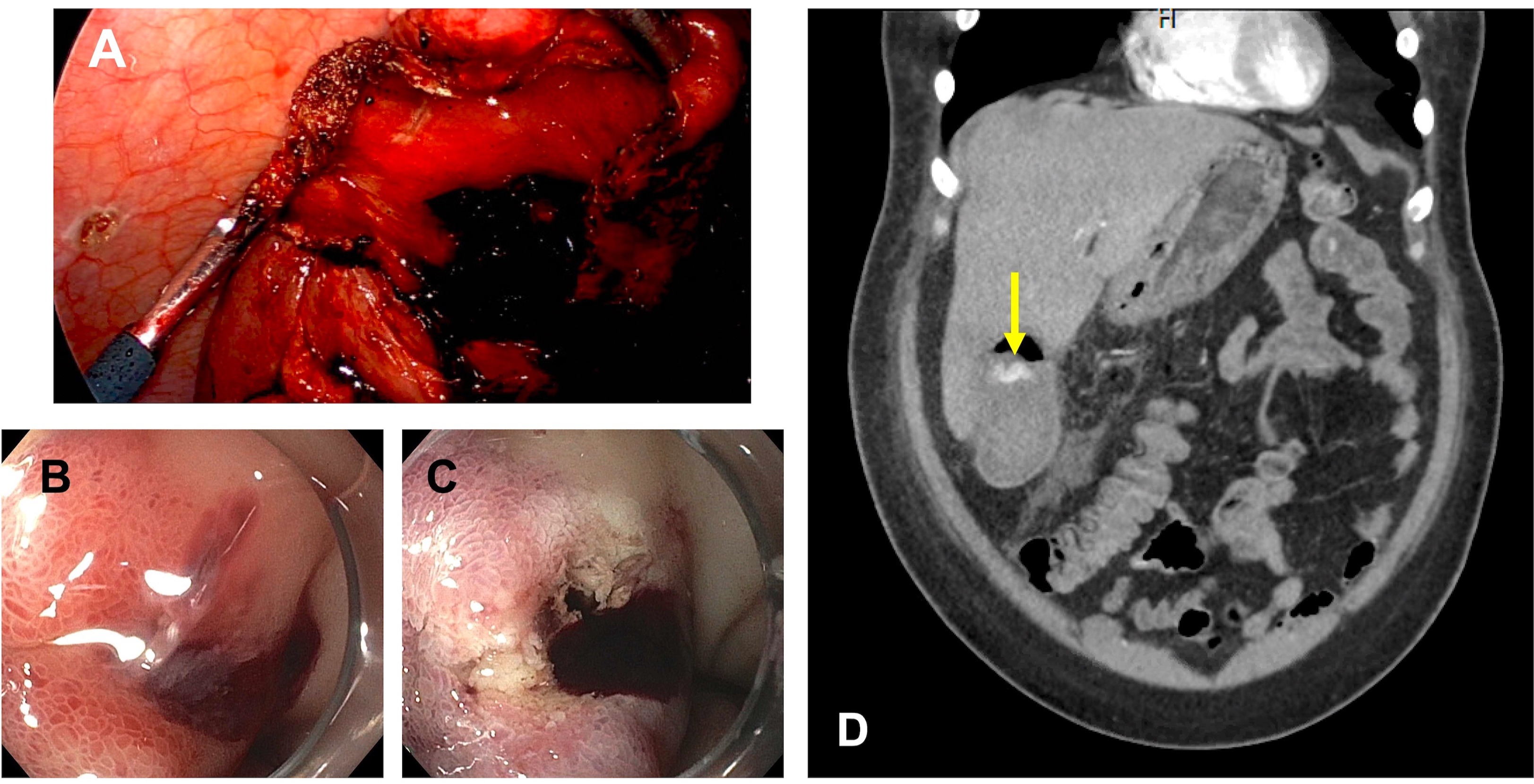
Case Description/Methods: A 43-year-old man with a past medical history of hypertension and paraplegia presented to the hospital with black tarry stools for 1 day. He denied fever, abdominal pain, and diarrhea. Vital signs were normal. Physical examination was significant for conjunctival pallor. Laboratory showed Hb 6g/dL, Hct 22.3%, WBC 8.20 k/µL, platelet 339 k/µL. The patient was transfused but continued to bleed and was taken to endoscopy. Further history revealed that the patient is T8 level paraplegic. Esophagogastroduodenoscopy showed a duodenal ulcer with oozing hemorrhage which was treated with thermotherapy; however, oozing continued, thermotherapy was avoided to prevent deep tissue injury and perforation as exact bleeding source could not be identified. Interventional radiology was consulted for embolization. After embolization, his hemoglobin continued to drop requiring blood transfusion. Computed tomography (CT) with angiography of the abdomen and pelvis was then performed which revealed a small focal area of active bleeding in the gallbladder. Patient was taken for emergent cholecystectomy. Intraoperative finding revealed active bleeding with clot in the gallbladder lumen. Following surgery, patient’s hemoglobin stabilized. Histopathology of the resected gallbladder revealed multiple stones impact in the gallbladder wall.
Discussion: Hemorrhagic cholecystitis is an extremely rare complication of cholecystitis. Our patient has no risk factor for developing hemorrhagic cholecystitis and his clinical presentation was ambiguous since the patient is paraplegic and does not have normal sensation in his abdomen. Patients with upper gastrointestinal bleeding (UGIB) usually undergo EGD for the management of the bleeding. However, UGIB refractory to an endoscopic treatment often requires endovascular intervention by radiology and surgery as appropriate. In our case CT angiogram of abdomen and pelvis revealed second source of the bleeding which was in the gallbladder leading to emergent cholecystectomy.This is a rare coincidence in which a patient with simultaneous bleeding from duodenal ulcer also found to have hemorrhagic cholecystitis. One hypothesis includes cholecystoduodenal (bilioenteric) fistula which is the infrequent complication of untreated cholelithiasis.
Disclosures:
Busara Songtanin, MD1, Kenneth Nugent, MD1, Kanak Das, MD2. C0346 - A Case of Hemorrhagic Cholecystitis and Bleeding Duodenal (Ulcer): A Rare Coincidence!, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Texas Tech University Health Sciences Center, Lubbock, TX; 2Texas Tech University Health Sciences Center and University Medical Center, Lubbock, TX
Introduction: Hemorrhagic cholecystitis is a life-threatening condition and may result in death if not treated promptly. Here, we present an atypical case of hemorrhagic cholecystitis that presented with melena but no abdominal pain.
Case Description/Methods: A 43-year-old man with a past medical history of hypertension and paraplegia presented to the hospital with black tarry stools for 1 day. He denied fever, abdominal pain, and diarrhea. Vital signs were normal. Physical examination was significant for conjunctival pallor. Laboratory showed Hb 6g/dL, Hct 22.3%, WBC 8.20 k/µL, platelet 339 k/µL. The patient was transfused but continued to bleed and was taken to endoscopy. Further history revealed that the patient is T8 level paraplegic. Esophagogastroduodenoscopy showed a duodenal ulcer with oozing hemorrhage which was treated with thermotherapy; however, oozing continued, thermotherapy was avoided to prevent deep tissue injury and perforation as exact bleeding source could not be identified. Interventional radiology was consulted for embolization. After embolization, his hemoglobin continued to drop requiring blood transfusion. Computed tomography (CT) with angiography of the abdomen and pelvis was then performed which revealed a small focal area of active bleeding in the gallbladder. Patient was taken for emergent cholecystectomy. Intraoperative finding revealed active bleeding with clot in the gallbladder lumen. Following surgery, patient’s hemoglobin stabilized. Histopathology of the resected gallbladder revealed multiple stones impact in the gallbladder wall.
Discussion: Hemorrhagic cholecystitis is an extremely rare complication of cholecystitis. Our patient has no risk factor for developing hemorrhagic cholecystitis and his clinical presentation was ambiguous since the patient is paraplegic and does not have normal sensation in his abdomen. Patients with upper gastrointestinal bleeding (UGIB) usually undergo EGD for the management of the bleeding. However, UGIB refractory to an endoscopic treatment often requires endovascular intervention by radiology and surgery as appropriate. In our case CT angiogram of abdomen and pelvis revealed second source of the bleeding which was in the gallbladder leading to emergent cholecystectomy.This is a rare coincidence in which a patient with simultaneous bleeding from duodenal ulcer also found to have hemorrhagic cholecystitis. One hypothesis includes cholecystoduodenal (bilioenteric) fistula which is the infrequent complication of untreated cholelithiasis.
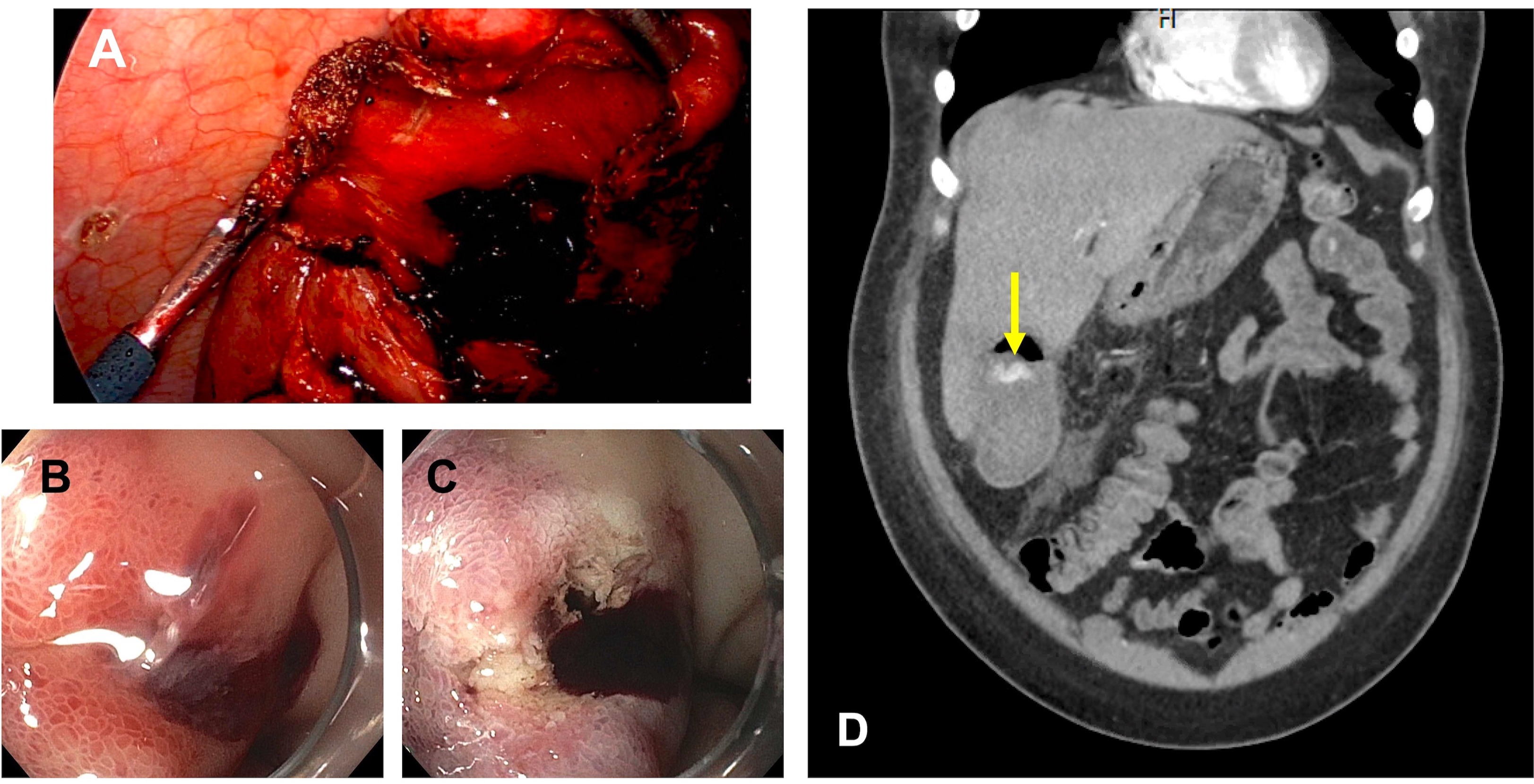
Figure: Figure 1 (A) Laparoscopic performed for total cholecystectomy showed actively bleed with clot in gall bladder lumen (B) EGD showed duodenal ulcer with oozing hemorrhage (C) Ongoing bleeding despite thermotherapy (D) CT angiography of abdomen and pelvis showed contrast extravasation in the gall bladder lumen (yellow arrow) suggesting active bleeding into gall bladder
Disclosures:
Busara Songtanin indicated no relevant financial relationships.
Kenneth Nugent indicated no relevant financial relationships.
Kanak Das indicated no relevant financial relationships.
Busara Songtanin, MD1, Kenneth Nugent, MD1, Kanak Das, MD2. C0346 - A Case of Hemorrhagic Cholecystitis and Bleeding Duodenal (Ulcer): A Rare Coincidence!, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
