Back

Poster Session B - Monday Morning
Category: Biliary/Pancreas
B0050 - Idiopathic Non-Caseating Pancreatic Granuloma Mimicking Neuroendocrine Tumor: A Challenging Diagnostic Dilemma
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
Antoine Boustany, MD, MPH
Cleveland Clinic Foundation
Cleveland, OH
Presenting Author(s)
Antoine Boustany, MD, MPH1, Eduard Krishtopaytis, MD1, Ashraf Almomani, MD1, Prabhat Kumar, MD1, Somtochukwu Onwuzo, MD1, Hassan M. Shaheen, MD1, Anfisa Baiandurova, MD2, Ala Abdel Jalil, MD1
1Cleveland Clinic Foundation, Cleveland, OH; 2Oregon Health & Science University, Portland, OR
Introduction: Pancreatic granuloma is rare. Caseating granuloma is usually caused by tuberculosis, while non-caseating granuloma is mainly secondary to systemic diseases such as sarcoidosis, rheumatoid arthritis, fungal infection, and Crohn’s disease. Idiopathic etiology can present a diagnostic challenge, requiring further investigation to differentiate it from malignancy. We present an interesting case of a patient who presented with a concern for a neuroendocrine tumor before diagnosing idiopathic non-caseating pancreatic granuloma.
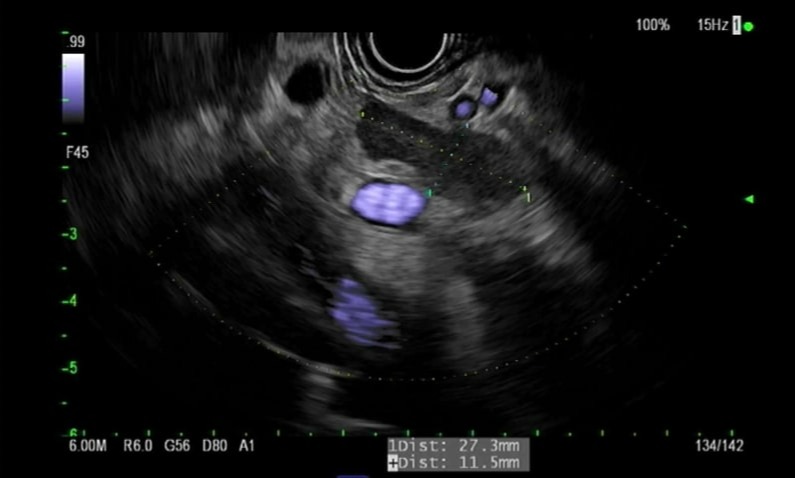
Case Description/Methods: A 75-year-old female presented with left upper quadrant pain, chronic diarrhea, and palpitations. The physical exam was unremarkable. Workup was significant for elevated serum chromogranin 3,123 ng/ml, with mildly elevated urine metanephrines. Magnetic resonance imaging showed a stable 2.5 cm cystic lesion in the tail of the pancreas communicating with the main pancreatic duct and hypointense area in the tail. 68Ga DOTATATE scan was negative for neuroendocrine tumor. Endoscopic ultrasound showed a multi-cystic lesion in the tail of the pancreas with thick septations consistent with branch-duct intrapapillary mucinous neoplasm (BD-IPMN), and a 2.7 cm homogenous well-defined hypoechoic area in the tail of pancreas along with multiple enlarged peripancreatic lymph nodes (Image 1). Fine needle biopsy showed multiple non-caseating granulomas with benign pancreatic and lymphoid tissue. There was no evidence of malignancy, and stains for acid-fast bacilli, FITE stain, and fungal cultures were negative. A benign idiopathic etiology was concluded. At the 6-months follow-up, the patient was doing well.
Discussion: Non-caseating pancreatic granuloma has been described in a few case reports. Sarcoidosis was the most common cause, followed by rheumatoid arthritis and Crohn’s disease. Other cases were associated with granulomatosis with polyangiitis (formerly Wegener's granulomatosis), xanthogranulomatous disease, insulin-dependent diabetes mellitus, or foreign body (Talc). Patients may present with epigastric pain, sometimes associated with weight loss, jaundice, fever, or nausea. Further workup and sampling, or even surgery, might be necessary before reaching a solid diagnosis and ruling out malignancy. Therefore, it is essential to rule out other etiologies before confirming the diagnosis of idiopathic pancreatic non-caseating granuloma.
Disclosures:
Antoine Boustany, MD, MPH1, Eduard Krishtopaytis, MD1, Ashraf Almomani, MD1, Prabhat Kumar, MD1, Somtochukwu Onwuzo, MD1, Hassan M. Shaheen, MD1, Anfisa Baiandurova, MD2, Ala Abdel Jalil, MD1. B0050 - Idiopathic Non-Caseating Pancreatic Granuloma Mimicking Neuroendocrine Tumor: A Challenging Diagnostic Dilemma, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Cleveland Clinic Foundation, Cleveland, OH; 2Oregon Health & Science University, Portland, OR
Introduction: Pancreatic granuloma is rare. Caseating granuloma is usually caused by tuberculosis, while non-caseating granuloma is mainly secondary to systemic diseases such as sarcoidosis, rheumatoid arthritis, fungal infection, and Crohn’s disease. Idiopathic etiology can present a diagnostic challenge, requiring further investigation to differentiate it from malignancy. We present an interesting case of a patient who presented with a concern for a neuroendocrine tumor before diagnosing idiopathic non-caseating pancreatic granuloma.
Case Description/Methods: A 75-year-old female presented with left upper quadrant pain, chronic diarrhea, and palpitations. The physical exam was unremarkable. Workup was significant for elevated serum chromogranin 3,123 ng/ml, with mildly elevated urine metanephrines. Magnetic resonance imaging showed a stable 2.5 cm cystic lesion in the tail of the pancreas communicating with the main pancreatic duct and hypointense area in the tail. 68Ga DOTATATE scan was negative for neuroendocrine tumor. Endoscopic ultrasound showed a multi-cystic lesion in the tail of the pancreas with thick septations consistent with branch-duct intrapapillary mucinous neoplasm (BD-IPMN), and a 2.7 cm homogenous well-defined hypoechoic area in the tail of pancreas along with multiple enlarged peripancreatic lymph nodes (Image 1). Fine needle biopsy showed multiple non-caseating granulomas with benign pancreatic and lymphoid tissue. There was no evidence of malignancy, and stains for acid-fast bacilli, FITE stain, and fungal cultures were negative. A benign idiopathic etiology was concluded. At the 6-months follow-up, the patient was doing well.
Discussion: Non-caseating pancreatic granuloma has been described in a few case reports. Sarcoidosis was the most common cause, followed by rheumatoid arthritis and Crohn’s disease. Other cases were associated with granulomatosis with polyangiitis (formerly Wegener's granulomatosis), xanthogranulomatous disease, insulin-dependent diabetes mellitus, or foreign body (Talc). Patients may present with epigastric pain, sometimes associated with weight loss, jaundice, fever, or nausea. Further workup and sampling, or even surgery, might be necessary before reaching a solid diagnosis and ruling out malignancy. Therefore, it is essential to rule out other etiologies before confirming the diagnosis of idiopathic pancreatic non-caseating granuloma.
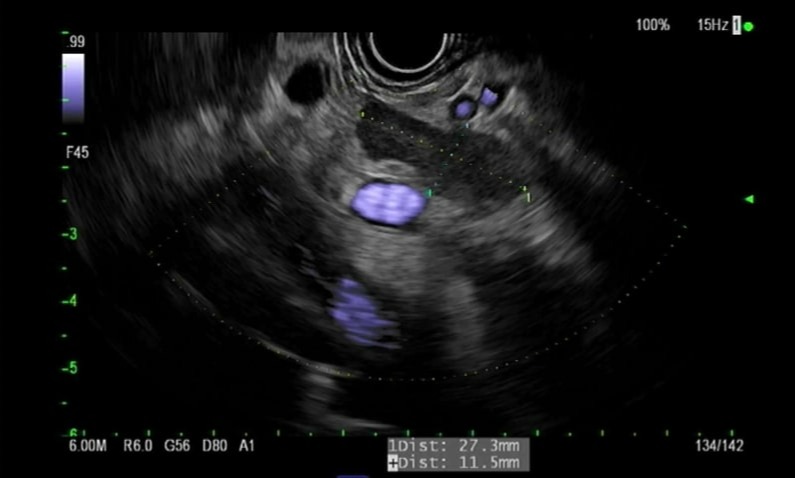
Figure: Image 1: Endoscopic ultrasound (EUS) showing a homogenous & well-defined hypoechoic mass in the tail of the pancreas, measuring 11 x 27 mm.
Disclosures:
Antoine Boustany indicated no relevant financial relationships.
Eduard Krishtopaytis indicated no relevant financial relationships.
Ashraf Almomani indicated no relevant financial relationships.
Prabhat Kumar indicated no relevant financial relationships.
Somtochukwu Onwuzo indicated no relevant financial relationships.
Hassan Shaheen indicated no relevant financial relationships.
Anfisa Baiandurova indicated no relevant financial relationships.
Ala Abdel Jalil indicated no relevant financial relationships.
Antoine Boustany, MD, MPH1, Eduard Krishtopaytis, MD1, Ashraf Almomani, MD1, Prabhat Kumar, MD1, Somtochukwu Onwuzo, MD1, Hassan M. Shaheen, MD1, Anfisa Baiandurova, MD2, Ala Abdel Jalil, MD1. B0050 - Idiopathic Non-Caseating Pancreatic Granuloma Mimicking Neuroendocrine Tumor: A Challenging Diagnostic Dilemma, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
