Back


Poster Session C - Monday Afternoon
Category: Colon
C0134 - A Rare Case of Submucosal Granular Cell Tumor Presenting as a Single Colon Polyp
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Has Audio

Talia F. Malik, MD
Chicago Medical School at Rosalind Franklin University of Medicine and Science
North Chicago, IL
Presenting Author(s)
Talia F. Malik, MD1, Pallavi Shah, MD2, Rupal Parmar, MD2
1Chicago Medical School at Rosalind Franklin University of Medicine and Science, North Chicago, IL; 2Captain James A. Lovell Federal Health Care Center, North Chicago, IL
Introduction: Granular cell tumor (GCT) is a soft tissue neoplasm that is known to originate from Schwann cells. It may occur anywhere in the body however only 5-11% arise within the gastrointestinal tract with the majority occurring within the esophagus. Rarely, GCT may arise in the colon mimicking a benign colon polyp. We present an unusual case of a patient diagnosed with a colonic submucosal GCT.
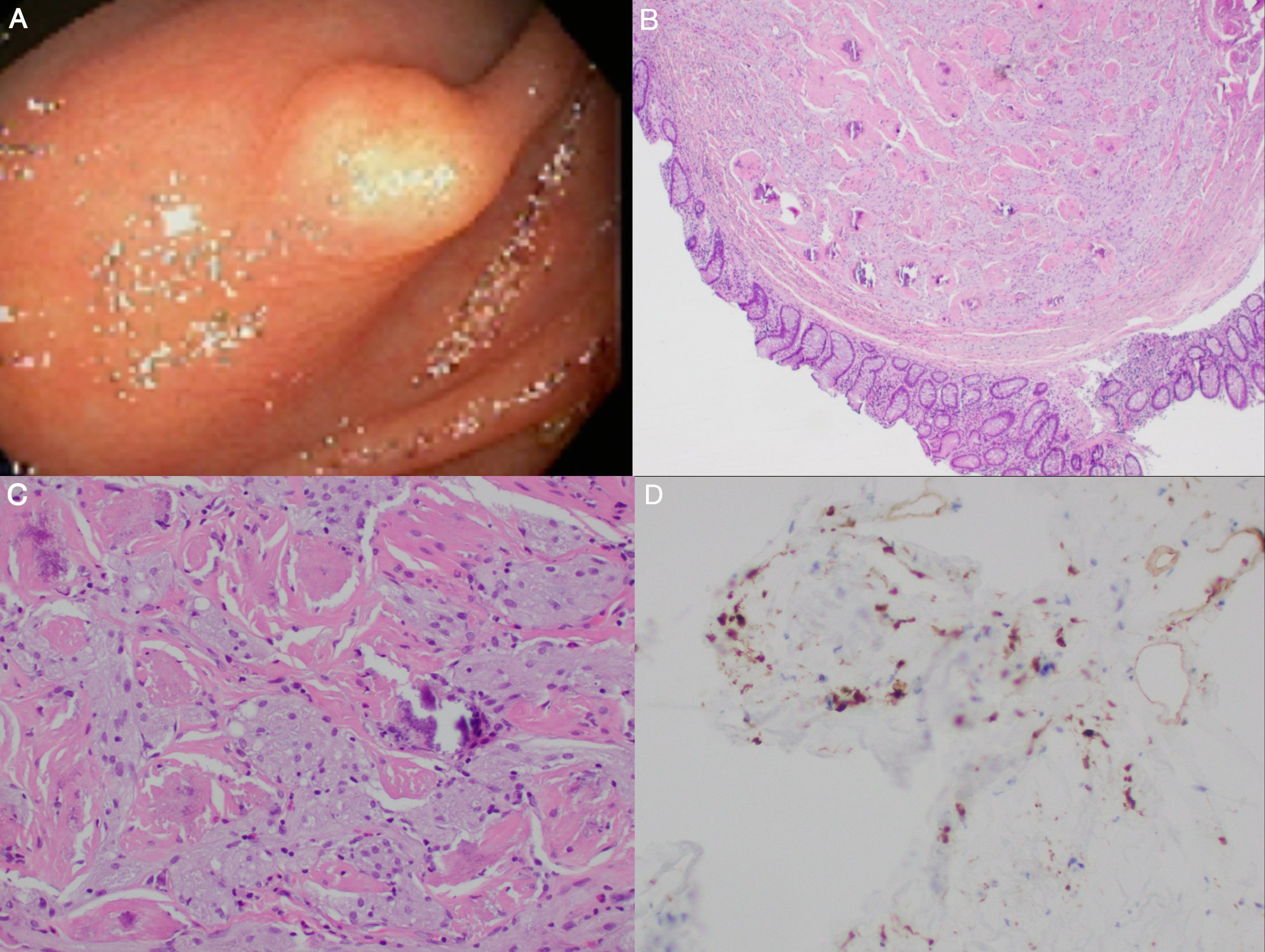
Case Description/Methods: A 61-year-old male with past history of gastroesophageal reflux disease presented with mild intermittent diffuse aching abdominal pain for the last 10 years. The patient reported a single episode of hematochezia at the time of symptom onset. Physical exam, laboratory studies, and imaging were largely unremarkable. Colonoscopy revealed an 8 mm firm submucosal nodule in the ascending colon (A). The lesion was completely resected using hot snare polypectomy. Histopathologic exam of the specimen revealed large polyclonal cells with abundant granular, eosinophilic cytoplasm and wavy nuclei (B, C). Immunohistochemical analysis confirmed the diagnosis of GCT by positive staining of S-100 (D) and CD68. The patient was scheduled for surveillance colonoscopy.
Discussion: GCT is most commonly seen in middle-aged women in the head, neck, skin, and subcutaneous tissues. 65% of gastrointestinal GCTs arise within the esophagus followed by the duodenum, anus, and stomach. Although the majority of GCTs are benign there is a 1-2% risk of malignancy. Malignant GCTs have a poor prognosis with a reported 3-year mortality of 60% with high rates of recurrence and metastasis. Colonic GCT is extremely rare with only 130 cases reported so far and its management has not been widely studied. Depending on tumor size and extent, complete resection with polypectomy vs endoscopic mucosal resection is the safest and recommended treatment for submucosal GCTs with follow-up colonoscopy. As the majority of colonic GCTs have a benign appearance on endoscopic examination, it’s important to follow up with histopathological analysis to differentiate it from other colonic lesions. Gastroenterologists should consider GCT in the differential diagnosis of submucosal colonic tumors.
Disclosures:
Talia F. Malik, MD1, Pallavi Shah, MD2, Rupal Parmar, MD2. C0134 - A Rare Case of Submucosal Granular Cell Tumor Presenting as a Single Colon Polyp, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Chicago Medical School at Rosalind Franklin University of Medicine and Science, North Chicago, IL; 2Captain James A. Lovell Federal Health Care Center, North Chicago, IL
Introduction: Granular cell tumor (GCT) is a soft tissue neoplasm that is known to originate from Schwann cells. It may occur anywhere in the body however only 5-11% arise within the gastrointestinal tract with the majority occurring within the esophagus. Rarely, GCT may arise in the colon mimicking a benign colon polyp. We present an unusual case of a patient diagnosed with a colonic submucosal GCT.
Case Description/Methods: A 61-year-old male with past history of gastroesophageal reflux disease presented with mild intermittent diffuse aching abdominal pain for the last 10 years. The patient reported a single episode of hematochezia at the time of symptom onset. Physical exam, laboratory studies, and imaging were largely unremarkable. Colonoscopy revealed an 8 mm firm submucosal nodule in the ascending colon (A). The lesion was completely resected using hot snare polypectomy. Histopathologic exam of the specimen revealed large polyclonal cells with abundant granular, eosinophilic cytoplasm and wavy nuclei (B, C). Immunohistochemical analysis confirmed the diagnosis of GCT by positive staining of S-100 (D) and CD68. The patient was scheduled for surveillance colonoscopy.
Discussion: GCT is most commonly seen in middle-aged women in the head, neck, skin, and subcutaneous tissues. 65% of gastrointestinal GCTs arise within the esophagus followed by the duodenum, anus, and stomach. Although the majority of GCTs are benign there is a 1-2% risk of malignancy. Malignant GCTs have a poor prognosis with a reported 3-year mortality of 60% with high rates of recurrence and metastasis. Colonic GCT is extremely rare with only 130 cases reported so far and its management has not been widely studied. Depending on tumor size and extent, complete resection with polypectomy vs endoscopic mucosal resection is the safest and recommended treatment for submucosal GCTs with follow-up colonoscopy. As the majority of colonic GCTs have a benign appearance on endoscopic examination, it’s important to follow up with histopathological analysis to differentiate it from other colonic lesions. Gastroenterologists should consider GCT in the differential diagnosis of submucosal colonic tumors.
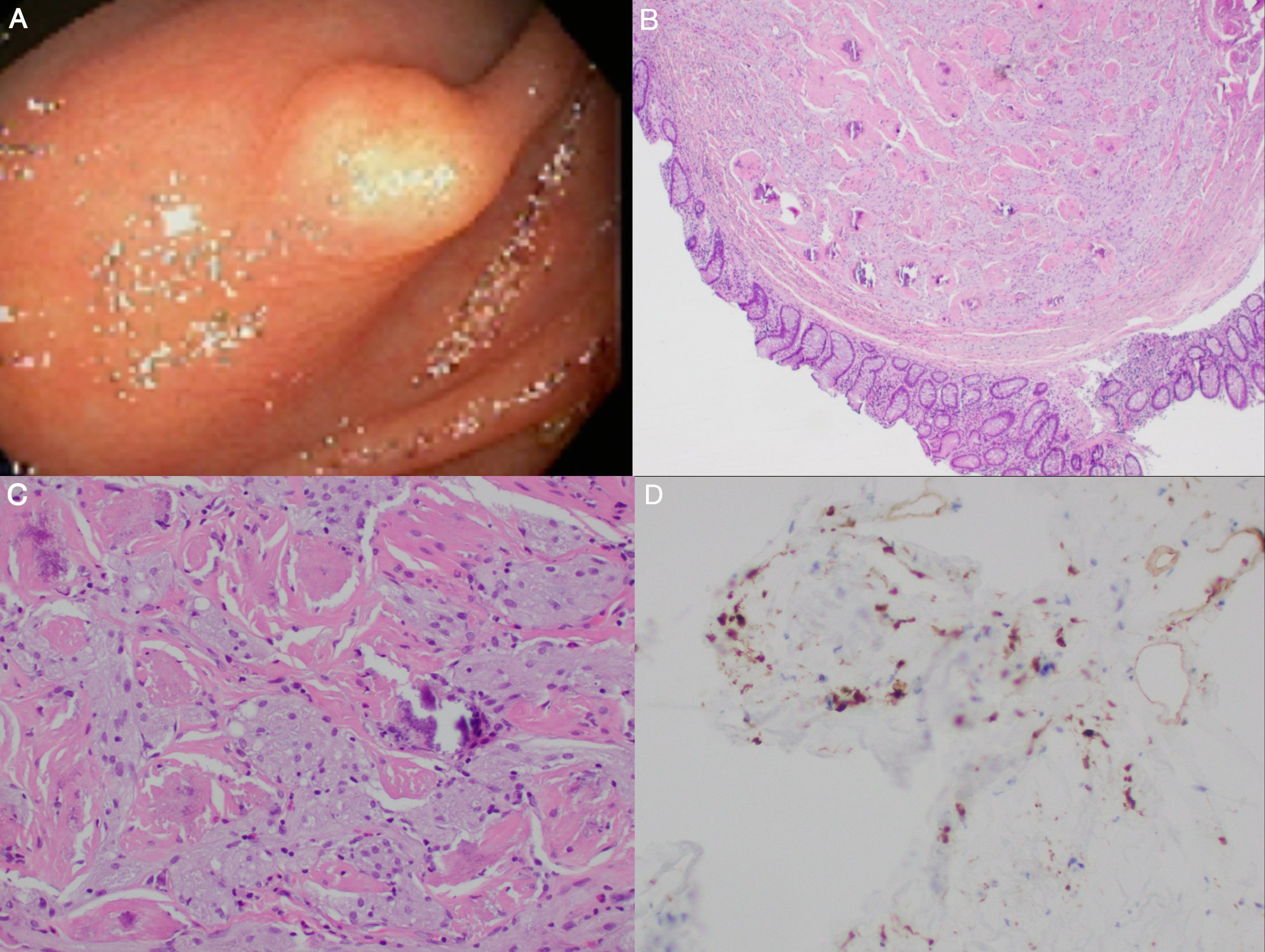
Figure: Figure 1. (A) Colonoscopy image of granular cell tumor in the ascending colon appearing as an 8 mm submucosal nodule. (B) H&E stain showing submucosal tumor covered with normal mucosa (magnification 40x). (C) H&E stain showing large polyclonal cells with abundant granular, eosinophilic cytoplasm and wavy nuclei (magnification 200x). (D) Immunohistochemical analysis showing positive staining of S-100 (magnification 200x).
Disclosures:
Talia Malik indicated no relevant financial relationships.
Pallavi Shah indicated no relevant financial relationships.
Rupal Parmar indicated no relevant financial relationships.
Talia F. Malik, MD1, Pallavi Shah, MD2, Rupal Parmar, MD2. C0134 - A Rare Case of Submucosal Granular Cell Tumor Presenting as a Single Colon Polyp, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
