Back
Poster Session C - Monday Afternoon
Category: IBD
C0382 - Dermatologic Manifestations in Patients With Inflammatory Bowel Disease
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
- MA
Motasem Alkhayyat, MD
Cleveland Clinic Foundation
Cleveland, Ohio
Presenting Author(s)
Almaza A. Albakri, MD1, Motasem Alkhayyat, MD2, Ashraf Almomani, MD2, Khaled Alsabbagh Alchirazi, MD3, Muhammad Sarmini, MD3, Prabhat Kumar, MD2, Antoine Boustany, MD, MPH2, Eduard Krishtopaytis, MD2, Dana Alshaikh, MD4, Mohammad Abureesh, MD5, Mohammad Zmaili, MD3, Rama Nanah, MD3, Feras Alkhalaileh, MD3, Eiman Wazwaz, PharmD6, Emad Mansoor, MD7, Miguel Regueiro, MD8
1Royal Jordanian Medical Services, Amman, Al Karak, Jordan; 2Cleveland Clinic Foundation, Cleveland, OH; 3Cleveland Clinic, Cleveland, OH; 4Mutah University, Amman, Al Karak, Jordan; 5Staten Island University Hospital, New York, NY; 6University of Jordan, Cleveland, OH; 7University Hospital Medical Center, Cleveland, OH; 8Cleveland Clinic Main Campus, Cleveland, OH
Introduction: There are several extraintestinal manifestations of inflammatory bowel disease (IBD) including cutaneous. Furthermore, new biologics have been also associated with cutaneous side effects. However, the prevalence of extraintestinal manifestations in patients with IBD and those who receive anti-tumor necrosis factors (anti-TNFs) have not been extensively studied. Using a large database, we sought to describe the rates of selected cutaneous manifestations of IBD as long as adverse effects of anti-TNFs.
Methods: We queried a multi-institutional database (Explorys Inc, Cleveland, OH, USA), an aggregate of electronic health record data from 26 US healthcare systems was surveyed. A cohort of patients with a Systematized Nomenclature of Medicine-Clinical Terms of inflammatory bowel disease between 2017-2021 was identified. Statistical analysis was performed using Statistical Package for Social Sciences (SPSS version 25, IBM Corp). For all analyses, a 2-sided P value of < 0.05 was considered statistically significant.
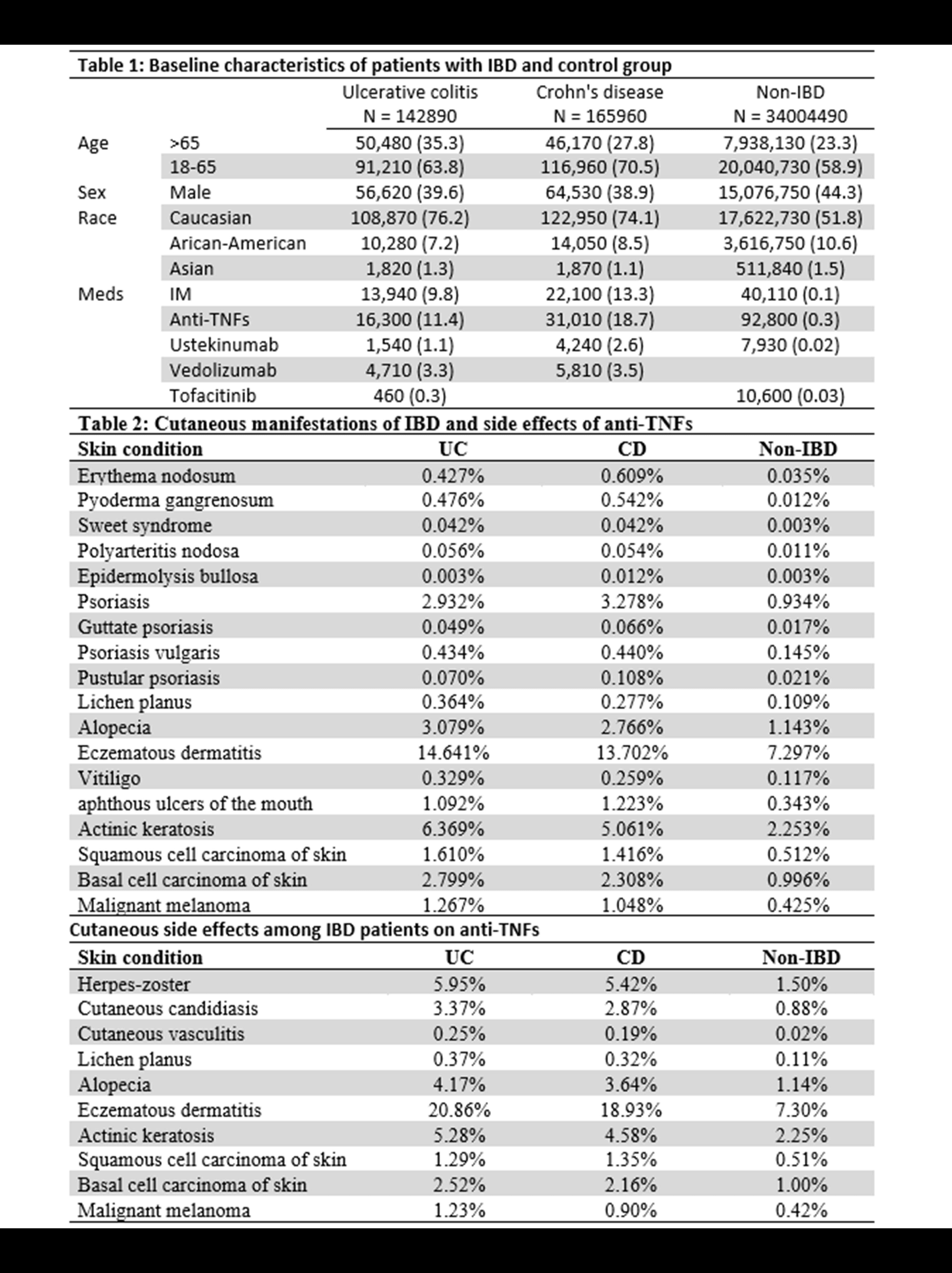
Results: Of the 34,277,840 individuals in the database, 142,890 (0.42%) and 165,960 (0.48%) had a diagnosis of ulcerative colitis (UC) and Crohn’s disease (CD) respectively. Baseline characteristics of patients with IBD and control group are shown in Table 1. Compared to the non-IBD group, patients with a history of IBD had a higher rates of multiple skin conditions including erythema nodosum, pyoderma gangrenosum, sweet syndrome, psoriasis, lichen planus, alopecia, eczema, vitiligo, bullous disease, and skin cancers. Among IBD patients, those who are on anti-TNFs and immunomodulator (IM) had higher rates of herpes/zoster and candida infections, lichen planus, alopecia, eczema and melanoma and non-melanoma skin cancers compared to anti-TNFs alone (Table 3).
Discussion: In this large database, we found a higher risk association between IBD and multiple skin conditions including skin cancers. Interesting, IBD patients treated with anti-TNFs had double rates of melanoma and non-melanoma skin cancers. Further epidemiological studies are required to validate these findings and increase attention to adequately screening for skin cancers and dermatology referral while taking care of IBD.
Disclosures:
Almaza A. Albakri, MD1, Motasem Alkhayyat, MD2, Ashraf Almomani, MD2, Khaled Alsabbagh Alchirazi, MD3, Muhammad Sarmini, MD3, Prabhat Kumar, MD2, Antoine Boustany, MD, MPH2, Eduard Krishtopaytis, MD2, Dana Alshaikh, MD4, Mohammad Abureesh, MD5, Mohammad Zmaili, MD3, Rama Nanah, MD3, Feras Alkhalaileh, MD3, Eiman Wazwaz, PharmD6, Emad Mansoor, MD7, Miguel Regueiro, MD8. C0382 - Dermatologic Manifestations in Patients With Inflammatory Bowel Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Royal Jordanian Medical Services, Amman, Al Karak, Jordan; 2Cleveland Clinic Foundation, Cleveland, OH; 3Cleveland Clinic, Cleveland, OH; 4Mutah University, Amman, Al Karak, Jordan; 5Staten Island University Hospital, New York, NY; 6University of Jordan, Cleveland, OH; 7University Hospital Medical Center, Cleveland, OH; 8Cleveland Clinic Main Campus, Cleveland, OH
Introduction: There are several extraintestinal manifestations of inflammatory bowel disease (IBD) including cutaneous. Furthermore, new biologics have been also associated with cutaneous side effects. However, the prevalence of extraintestinal manifestations in patients with IBD and those who receive anti-tumor necrosis factors (anti-TNFs) have not been extensively studied. Using a large database, we sought to describe the rates of selected cutaneous manifestations of IBD as long as adverse effects of anti-TNFs.
Methods: We queried a multi-institutional database (Explorys Inc, Cleveland, OH, USA), an aggregate of electronic health record data from 26 US healthcare systems was surveyed. A cohort of patients with a Systematized Nomenclature of Medicine-Clinical Terms of inflammatory bowel disease between 2017-2021 was identified. Statistical analysis was performed using Statistical Package for Social Sciences (SPSS version 25, IBM Corp). For all analyses, a 2-sided P value of < 0.05 was considered statistically significant.
Results: Of the 34,277,840 individuals in the database, 142,890 (0.42%) and 165,960 (0.48%) had a diagnosis of ulcerative colitis (UC) and Crohn’s disease (CD) respectively. Baseline characteristics of patients with IBD and control group are shown in Table 1. Compared to the non-IBD group, patients with a history of IBD had a higher rates of multiple skin conditions including erythema nodosum, pyoderma gangrenosum, sweet syndrome, psoriasis, lichen planus, alopecia, eczema, vitiligo, bullous disease, and skin cancers. Among IBD patients, those who are on anti-TNFs and immunomodulator (IM) had higher rates of herpes/zoster and candida infections, lichen planus, alopecia, eczema and melanoma and non-melanoma skin cancers compared to anti-TNFs alone (Table 3).
Discussion: In this large database, we found a higher risk association between IBD and multiple skin conditions including skin cancers. Interesting, IBD patients treated with anti-TNFs had double rates of melanoma and non-melanoma skin cancers. Further epidemiological studies are required to validate these findings and increase attention to adequately screening for skin cancers and dermatology referral while taking care of IBD.
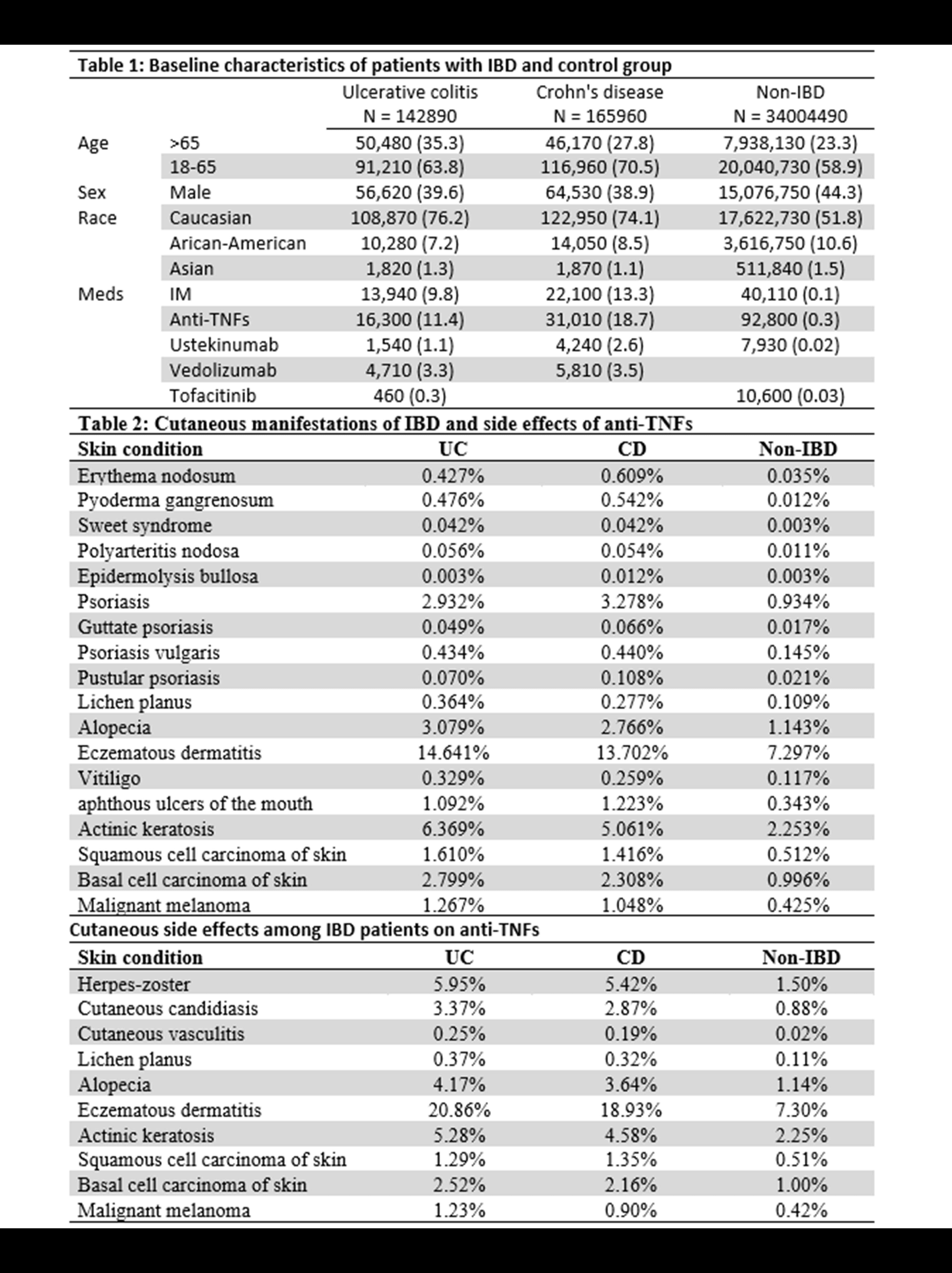
Figure: Tables 1,2,3
Disclosures:
Almaza Albakri indicated no relevant financial relationships.
Motasem Alkhayyat indicated no relevant financial relationships.
Ashraf Almomani indicated no relevant financial relationships.
Khaled Alsabbagh Alchirazi indicated no relevant financial relationships.
Muhammad Sarmini indicated no relevant financial relationships.
Prabhat Kumar indicated no relevant financial relationships.
Antoine Boustany indicated no relevant financial relationships.
Eduard Krishtopaytis indicated no relevant financial relationships.
Dana Alshaikh indicated no relevant financial relationships.
Mohammad Abureesh indicated no relevant financial relationships.
Mohammad Zmaili indicated no relevant financial relationships.
Rama Nanah indicated no relevant financial relationships.
Feras Alkhalaileh indicated no relevant financial relationships.
Eiman Wazwaz indicated no relevant financial relationships.
Emad Mansoor indicated no relevant financial relationships.
Miguel Regueiro: Abbvie – Advisory Committee/Board Member, Consultant. Abbvie – Grant/Research Support. ALFASIGMA, S.p.A. – Advisory Committee/Board Member. Allergan – Advisory Committee/Board Member. Amgen – Advisory Committee/Board Member. BMS – Grant/Research Support. Bristol Meyer Squibb – Advisory Committee/Board Member, Consultant. CC360 – Royalties. Celgene – Advisory Committee/Board Member. CME Outfitters – CME Companies. Cornerstones – CME Companies. Crohn’s and Colitis Foundation as Editor-in-Chief – Royalties. Genentech – Advisory Committee/Board Member. Genentech – Grant/Research Support. Gilead – Advisory Committee/Board Member. Gilead – Grant/Research Support. HMPGlobal – CME Companies. Imedex, GI Health Foundation (GiHF) – CME Companies. Janssen – Advisory Committee/Board Member, Consultant. Janssen – Grant/Research Support. Lilly – Grant/Research Support. MDEducation – CME Companies. Medscape – CME Companies. Miraca Labs – Advisory Committee/Board Member. MJH life sciences – CME Companies. Pfizer – Advisory Committee/Board Member, Consultant. Prometheus – Advisory Committee/Board Member. Remedy – CME Companies. Salix – Advisory Committee/Board Member. Seres – Advisory Committee/Board Member. Takeda – Advisory Committee/Board Member, Consultant. TARGET Pharma Solutions – Advisory Committee/Board Member. UCB – Grant/Research Support. WebMD – CME Companies. Wolters Kluwer Health as Author/Editor of UpToDate – Royalties.
Almaza A. Albakri, MD1, Motasem Alkhayyat, MD2, Ashraf Almomani, MD2, Khaled Alsabbagh Alchirazi, MD3, Muhammad Sarmini, MD3, Prabhat Kumar, MD2, Antoine Boustany, MD, MPH2, Eduard Krishtopaytis, MD2, Dana Alshaikh, MD4, Mohammad Abureesh, MD5, Mohammad Zmaili, MD3, Rama Nanah, MD3, Feras Alkhalaileh, MD3, Eiman Wazwaz, PharmD6, Emad Mansoor, MD7, Miguel Regueiro, MD8. C0382 - Dermatologic Manifestations in Patients With Inflammatory Bowel Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
