Back

Poster Session A - Sunday Afternoon
Category: Biliary/Pancreas
A0072 - Digesting a Differential of Zebras in a Unique Case of Pancreatitis
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Ryan K. Mui, DO, PhD
McLaren Greater Lansing
Lansing, Michigan
Presenting Author(s)
Ryan K. Mui, DO, PhD, Christopher White, DO, Christian H. Whitfield, DO, Soha Afzal, DO, Lauren A. Lyssy, DO, Justin Kisaka, DO
McLaren Greater Lansing, Lansing, MI
Introduction: While acute pancreatitis is often gallstone or alcohol related, initial workup usually includes consideration of medications, triglyceride level, malignancy, and autoimmune pancreatitis. There remains however a list of rare causes that is often overlooked and misdiagnosed as idiopathic. This is unfortunate and may delay potentially life-saving therapy. Here, we present a unique case of acute pancreatitis seropositive for lupus and mumps that spiraled into lupus cerebritis.
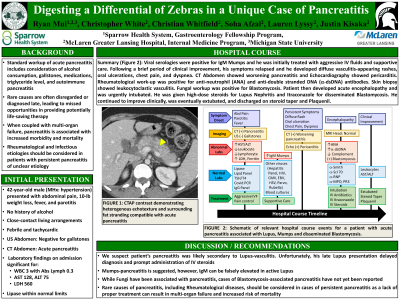
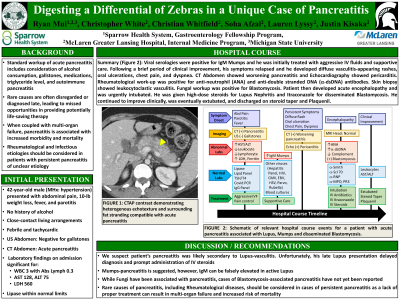
Case Description/Methods: A 42-year old male (PMHx. Hypertension) presented with a 6-week history of abdominal pain, weight loss, fever, parotitis and odynophagia. History was significant for close-contact confinement and negative for alcohol use. He was febrile and tachycardic. US was negative for gallstones. CTA showed acute pancreatitis. Labs were significant for WBC 3.21 (abs lymph 0.29), AST 128/ALT 75. Lipase, TSH, lipid panel, and IgG panel was unremarkable. An extensive viral panel was ordered and positive for mumps IgM. He was aggressively fluid resuscitated and developed clinical improvement throughout the week before an unexpected relapse of his symptoms. Over the next few weeks, he developed erythematous and vasculitic appearing rashes, arthralgias, oral ulcers, pericarditis, and eventually acute encephalopathy that required intubation. Skin biopsy showed leukocytoclastic vasculitis and connective tissue disease panel was positive for anti-dsDNA and ANA. He was started on high-dose pulse steroids for lupus cerebritis with remarkable improvement.
Discussion: We present a unique case of lupus-pancreatitis in a patient without any prior history. He was seropositive for mumps, which we ordered due to his history. However, mumps-pancreatitis is rare and usually mild. Interestingly, his clinical deterioration coincided with clinical features and serology consistent with lupus. Lupus can falsely elevate mumps IgM and his pancreatitis was likely from lupus-related vasculitis. Lupus-pancreatitis is uncommon and typically presents during lupus flares. To our knowledge, this is the first report of acute pancreatitis as an initial presentation of lupus cerebritis. Lupus-pancreatitis responds to prompt administration of IV steroids. Unfortunately, our patient’s late lupus presentation delayed immunotherapy. Therefore, we recommend consideration of connective tissue diseases in the autoimmune workup of persistent or relapsing pancreatitis.
Disclosures:
Ryan K. Mui, DO, PhD, Christopher White, DO, Christian H. Whitfield, DO, Soha Afzal, DO, Lauren A. Lyssy, DO, Justin Kisaka, DO. A0072 - Digesting a Differential of Zebras in a Unique Case of Pancreatitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
McLaren Greater Lansing, Lansing, MI
Introduction: While acute pancreatitis is often gallstone or alcohol related, initial workup usually includes consideration of medications, triglyceride level, malignancy, and autoimmune pancreatitis. There remains however a list of rare causes that is often overlooked and misdiagnosed as idiopathic. This is unfortunate and may delay potentially life-saving therapy. Here, we present a unique case of acute pancreatitis seropositive for lupus and mumps that spiraled into lupus cerebritis.
Case Description/Methods: A 42-year old male (PMHx. Hypertension) presented with a 6-week history of abdominal pain, weight loss, fever, parotitis and odynophagia. History was significant for close-contact confinement and negative for alcohol use. He was febrile and tachycardic. US was negative for gallstones. CTA showed acute pancreatitis. Labs were significant for WBC 3.21 (abs lymph 0.29), AST 128/ALT 75. Lipase, TSH, lipid panel, and IgG panel was unremarkable. An extensive viral panel was ordered and positive for mumps IgM. He was aggressively fluid resuscitated and developed clinical improvement throughout the week before an unexpected relapse of his symptoms. Over the next few weeks, he developed erythematous and vasculitic appearing rashes, arthralgias, oral ulcers, pericarditis, and eventually acute encephalopathy that required intubation. Skin biopsy showed leukocytoclastic vasculitis and connective tissue disease panel was positive for anti-dsDNA and ANA. He was started on high-dose pulse steroids for lupus cerebritis with remarkable improvement.
Discussion: We present a unique case of lupus-pancreatitis in a patient without any prior history. He was seropositive for mumps, which we ordered due to his history. However, mumps-pancreatitis is rare and usually mild. Interestingly, his clinical deterioration coincided with clinical features and serology consistent with lupus. Lupus can falsely elevate mumps IgM and his pancreatitis was likely from lupus-related vasculitis. Lupus-pancreatitis is uncommon and typically presents during lupus flares. To our knowledge, this is the first report of acute pancreatitis as an initial presentation of lupus cerebritis. Lupus-pancreatitis responds to prompt administration of IV steroids. Unfortunately, our patient’s late lupus presentation delayed immunotherapy. Therefore, we recommend consideration of connective tissue diseases in the autoimmune workup of persistent or relapsing pancreatitis.
Disclosures:
Ryan Mui indicated no relevant financial relationships.
Christopher White indicated no relevant financial relationships.
Christian Whitfield indicated no relevant financial relationships.
Soha Afzal indicated no relevant financial relationships.
Lauren Lyssy indicated no relevant financial relationships.
Justin Kisaka indicated no relevant financial relationships.
Ryan K. Mui, DO, PhD, Christopher White, DO, Christian H. Whitfield, DO, Soha Afzal, DO, Lauren A. Lyssy, DO, Justin Kisaka, DO. A0072 - Digesting a Differential of Zebras in a Unique Case of Pancreatitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
