Back

Poster Session C - Monday Afternoon
Category: GI Bleeding
C0353 - Back to Basics: A Case of Refractory Obscure Gastrointestinal Bleeding Due to Jejunal Leiomyoma
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

David N. Oakland, BS
Virginia Tech Carilion
Roanoke, Virginia
Presenting Author(s)
David N. Oakland, BS1, Sarah Schimming, DO2, Shravani Reddy, MD2, Robert D. Moylan, MD, PhD1
1Virginia Tech Carilion, Roanoke, VA; 2Virginia Tech Carilion School of Medicine, Roanoke, VA
Introduction: In the context of an acute gastrointestinal (GI) bleed, endoscopy is often first line as it allows for both diagnostic and therapeutic interventions. In comparison to non-invasive imaging techniques, such as red blood cell (RBC) scintigraphy or computed tomography angiography (CTA), colonoscopy and esophagogastroduodenoscopy (EGD) allow for direct visualization and treatment. However, in the case of obscure GI bleeding, imaging is a valuable tool in a gastroenterologist’s arsenal and may guide therapeutic intervention. We present a case of refractory, obscure GI bleeding due to a large jejunal leiomyoma.
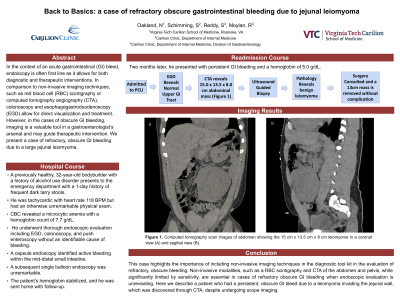
Case Description/Methods: A previously healthy 32-year-old man was admitted from the emergency department due to rectal bleeding and anemia. CBC revealed a microcytic anemia with a hemoglobin level of 7.7 g/dL. The patient was physically active with a history of heavy alcohol use. He underwent thorough endoscopic evaluation including EGD, colonoscopy, and push enteroscopy without an identifiable cause of bleeding. A capsule endoscopy identified active bleeding within the mid-distal small intestine. A subsequent single balloon endoscopy was unremarkable. The patient’s hemoglobin stabilized, and he was sent home with follow-up. Two months later, he presented with persistent GI bleeding and a hemoglobin of 5.0 g/dL. At this time, a CTA of the abdomen and pelvis revealed a 15 cm x 13.5 cm x 8 cm left-sided abdominal mass adjacent to the jejunum (Image). Ultrasound guided biopsy confirmed the diagnosis of a leiomyoma. Due to recurrent bleeding and the extent of the mass, he underwent surgical resection and recovered without incident.
Discussion: This case highlights the importance of including non-invasive imaging techniques in the diagnostic tool kit in the evaluation of refractory, obscure bleeding. Non-invasive modalities, such as a RBC scintigraphy and CTA of the abdomen and pelvis, while significantly limited by sensitivity, are essential in cases of refractory obscure GI bleeding when endoscopic evaluation is unrevealing. Here we describe a patient who had a persistent, obscure GI bleed due to a leiomyoma invading the jejunal wall, which was discovered through CTA, despite undergoing scope imaging.

Disclosures:
David N. Oakland, BS1, Sarah Schimming, DO2, Shravani Reddy, MD2, Robert D. Moylan, MD, PhD1. C0353 - Back to Basics: A Case of Refractory Obscure Gastrointestinal Bleeding Due to Jejunal Leiomyoma, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Virginia Tech Carilion, Roanoke, VA; 2Virginia Tech Carilion School of Medicine, Roanoke, VA
Introduction: In the context of an acute gastrointestinal (GI) bleed, endoscopy is often first line as it allows for both diagnostic and therapeutic interventions. In comparison to non-invasive imaging techniques, such as red blood cell (RBC) scintigraphy or computed tomography angiography (CTA), colonoscopy and esophagogastroduodenoscopy (EGD) allow for direct visualization and treatment. However, in the case of obscure GI bleeding, imaging is a valuable tool in a gastroenterologist’s arsenal and may guide therapeutic intervention. We present a case of refractory, obscure GI bleeding due to a large jejunal leiomyoma.
Case Description/Methods: A previously healthy 32-year-old man was admitted from the emergency department due to rectal bleeding and anemia. CBC revealed a microcytic anemia with a hemoglobin level of 7.7 g/dL. The patient was physically active with a history of heavy alcohol use. He underwent thorough endoscopic evaluation including EGD, colonoscopy, and push enteroscopy without an identifiable cause of bleeding. A capsule endoscopy identified active bleeding within the mid-distal small intestine. A subsequent single balloon endoscopy was unremarkable. The patient’s hemoglobin stabilized, and he was sent home with follow-up. Two months later, he presented with persistent GI bleeding and a hemoglobin of 5.0 g/dL. At this time, a CTA of the abdomen and pelvis revealed a 15 cm x 13.5 cm x 8 cm left-sided abdominal mass adjacent to the jejunum (Image). Ultrasound guided biopsy confirmed the diagnosis of a leiomyoma. Due to recurrent bleeding and the extent of the mass, he underwent surgical resection and recovered without incident.
Discussion: This case highlights the importance of including non-invasive imaging techniques in the diagnostic tool kit in the evaluation of refractory, obscure bleeding. Non-invasive modalities, such as a RBC scintigraphy and CTA of the abdomen and pelvis, while significantly limited by sensitivity, are essential in cases of refractory obscure GI bleeding when endoscopic evaluation is unrevealing. Here we describe a patient who had a persistent, obscure GI bleed due to a leiomyoma invading the jejunal wall, which was discovered through CTA, despite undergoing scope imaging.

Figure: Computed tomography scan images of abdomen showing the 15 cm x 13.5 cm x 8 cm leiomyoma in a coronal view (A) and sagittal view (B).
Disclosures:
David Oakland indicated no relevant financial relationships.
Sarah Schimming indicated no relevant financial relationships.
Shravani Reddy indicated no relevant financial relationships.
Robert Moylan indicated no relevant financial relationships.
David N. Oakland, BS1, Sarah Schimming, DO2, Shravani Reddy, MD2, Robert D. Moylan, MD, PhD1. C0353 - Back to Basics: A Case of Refractory Obscure Gastrointestinal Bleeding Due to Jejunal Leiomyoma, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
