Back

Poster Session B - Monday Morning
Category: Small Intestine
B0675 - Ethacrynic Acid-Associated Seronegative Enteropathy
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Kavya M. Reddy, MD
University of California Los Angeles David Geffen School of Medicine
Los Angeles, CA
Presenting Author(s)
Kavya M. Reddy, MD1, Michelle Hwang, MD1, Samuel French, MD, PhD2, Guy A. Weiss, MD3
1University of California Los Angeles David Geffen School of Medicine, Torrance, CA; 2University of California Los Angeles David Geffen School of Medicine, Los Angeles, CA; 3University of California Los Angeles, Los Angeles, CA
Introduction: Seronegative enteropathy is defined as negative serological celiac disease (CeD) testing, i.e., tissue transglutaminase (tTG), deaminated gliadin peptide (DGP), anti-endomysial antibody (EMA), in patients with villous atrophy on small bowel biopsies. Many common medications have been implicated in causing a reversible enteropathy, mainly olmesartan. We describe the first case of a patient who developed severe diarrhea and subsequent diagnosis of seronegative enteropathy following initiation of ethacrynic acid.
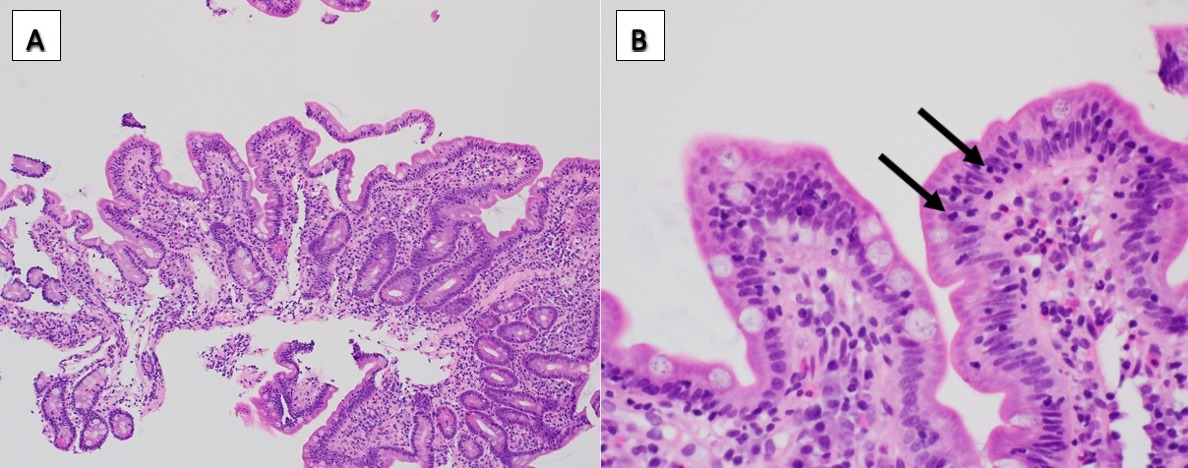
Case Description/Methods: A 78-year-old male with a history of hypertension, hyperlipidemia, and chronic kidney disease presented for outpatient gastroenterology consultation with a complaint of 16 days of moderate volume, watery stools occurring 3-5 times per day. He was started on ethacrynic acid by his nephrologist for volume overload approximately 6 weeks prior to presentation. He was also taking magnesium, vitamin E and vitamin C supplements, which he stopped, without improvement in diarrhea. He continued to take losartan for high blood pressure, which he had been on for many years. Infectious and chronic diarrhea workup returned negative except for an elevated calprotectin level (753 ug/g; normal < 49 ug/g). Colonoscopy and ileoscopy were normal, with negative random biopsies for microscopic colitis. Upper endoscopy was normal, however duodenal biopsies showed mild to moderate villous blunting (Figure 1a) and increased intraepithelial lymphocytes (Figure 1b), consistent with a Marsh 3a-3b lesion. CeD serological testing were normal with subsequently absent HLA DQ2 and DQ8. After stopping ethacrynic acid, the patient’s diarrhea resolved within 2 days and repeat duodenal biopsies 5 months later showed resolution of his enteropathy.
Discussion: Seronegative enteropathy is a clinical challenge as many conditions and medications may cause severe small intestinal damage. Seronegative celiac disease was excluded in this patient as his celiac genes were absent and his enteropathy resolved without a gluten-free diet. This is the first case to our knowledge of seronegative enteropathy associated with ethacrynic acid, with clinical and histological remission upon drug discontinuation. It is important for clinicians to recognize each potential drug associated with seronegative enteropathy, in order to properly diagnose and manage an easily reversible condition. Incorrect interpretation of the duodenal biopsies could have led to a misdiagnosis of CeD and an unnecessary gluten free diet.
Disclosures:
Kavya M. Reddy, MD1, Michelle Hwang, MD1, Samuel French, MD, PhD2, Guy A. Weiss, MD3. B0675 - Ethacrynic Acid-Associated Seronegative Enteropathy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of California Los Angeles David Geffen School of Medicine, Torrance, CA; 2University of California Los Angeles David Geffen School of Medicine, Los Angeles, CA; 3University of California Los Angeles, Los Angeles, CA
Introduction: Seronegative enteropathy is defined as negative serological celiac disease (CeD) testing, i.e., tissue transglutaminase (tTG), deaminated gliadin peptide (DGP), anti-endomysial antibody (EMA), in patients with villous atrophy on small bowel biopsies. Many common medications have been implicated in causing a reversible enteropathy, mainly olmesartan. We describe the first case of a patient who developed severe diarrhea and subsequent diagnosis of seronegative enteropathy following initiation of ethacrynic acid.
Case Description/Methods: A 78-year-old male with a history of hypertension, hyperlipidemia, and chronic kidney disease presented for outpatient gastroenterology consultation with a complaint of 16 days of moderate volume, watery stools occurring 3-5 times per day. He was started on ethacrynic acid by his nephrologist for volume overload approximately 6 weeks prior to presentation. He was also taking magnesium, vitamin E and vitamin C supplements, which he stopped, without improvement in diarrhea. He continued to take losartan for high blood pressure, which he had been on for many years. Infectious and chronic diarrhea workup returned negative except for an elevated calprotectin level (753 ug/g; normal < 49 ug/g). Colonoscopy and ileoscopy were normal, with negative random biopsies for microscopic colitis. Upper endoscopy was normal, however duodenal biopsies showed mild to moderate villous blunting (Figure 1a) and increased intraepithelial lymphocytes (Figure 1b), consistent with a Marsh 3a-3b lesion. CeD serological testing were normal with subsequently absent HLA DQ2 and DQ8. After stopping ethacrynic acid, the patient’s diarrhea resolved within 2 days and repeat duodenal biopsies 5 months later showed resolution of his enteropathy.
Discussion: Seronegative enteropathy is a clinical challenge as many conditions and medications may cause severe small intestinal damage. Seronegative celiac disease was excluded in this patient as his celiac genes were absent and his enteropathy resolved without a gluten-free diet. This is the first case to our knowledge of seronegative enteropathy associated with ethacrynic acid, with clinical and histological remission upon drug discontinuation. It is important for clinicians to recognize each potential drug associated with seronegative enteropathy, in order to properly diagnose and manage an easily reversible condition. Incorrect interpretation of the duodenal biopsies could have led to a misdiagnosis of CeD and an unnecessary gluten free diet.
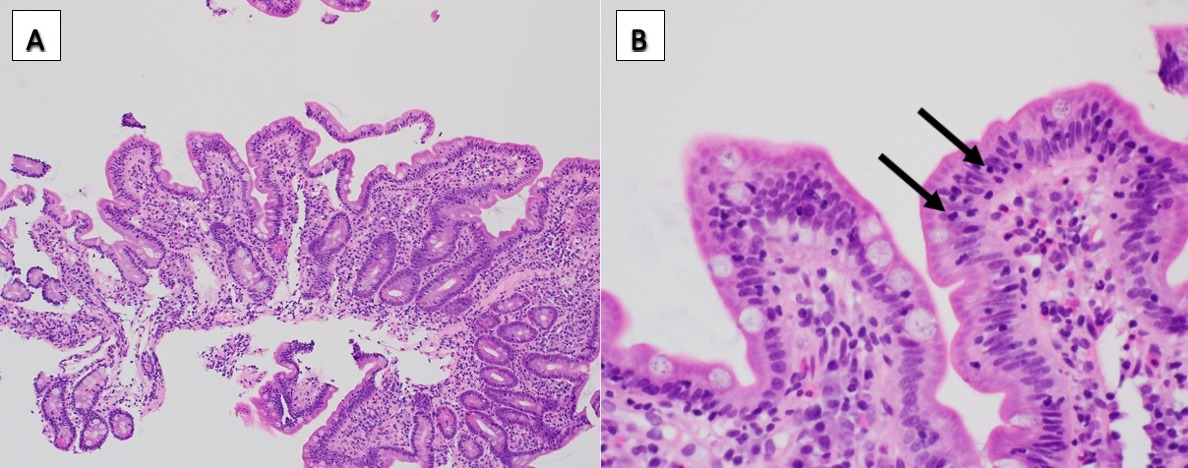
Figure: Figure 1: A: Duodenal biopsies showing villous blunting (H&E stain,100x magnification); B: Duodenal biopsies with arrows pointing to increased intraepithelial lymphocytes (H&E stain, 400x magnification)
Disclosures:
Kavya Reddy indicated no relevant financial relationships.
Michelle Hwang indicated no relevant financial relationships.
Samuel French indicated no relevant financial relationships.
Guy Weiss: EverlyHealth – Advisory Committee/Board Member.
Kavya M. Reddy, MD1, Michelle Hwang, MD1, Samuel French, MD, PhD2, Guy A. Weiss, MD3. B0675 - Ethacrynic Acid-Associated Seronegative Enteropathy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
