Back

Poster Session B - Monday Morning
Category: Stomach
B0728 - An Unusual Culprit for Gastric Ulceration
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Mohammad T. Sultan, DO, MS
Ochsner Clinic Foundation
New Orleans, LA
Presenting Author(s)
Mohammad T. Sultan, DO, MS, Luke Townsend, MD, Matthew Rice, MD
Ochsner Clinic Foundation, New Orleans, LA
Introduction: Actinomycosis is a chronic granulomatous disease caused by an anaerobic, gram positive, filamentous bacterium. Actinomycetes are commensal oral/intestinal bacteria that can manifest with fibrosis/necrosis, abscess formation, draining sinuses and fistulas when they invade susceptible tissue. Infection commonly affects the cervicofacial region (50%), however the literature describes abdominal involvement in 20% of cases (typically localized in the appendix and ileocecum). We describe a case of gastric ulceration secondary to actinomycosis.
Case Description/Methods: A 33-year-old female with Type 1 Diabetes Mellitus status post kidney-pancreas transplant on immunosuppression presents with one month of progressive, diffuse abdominal pain. Initial evaluation revealed acute renal failure of unclear etiology (creatinine of 5 from baseline of 1). Kidney biopsy revealed acute antibody mediated cellular rejection with donor specific antibodies. Methylprednisolone, PLEX and thymoglobulin were started. The patient’s ongoing rigors and abdominal pain prompted an infectious workup. Blood cultures returned with Group B Strep and Computed Tomography (CT) abdomen/pelvis without contrast showed diffuse gastric wall thickening and effacement of the gastric rugal folds.
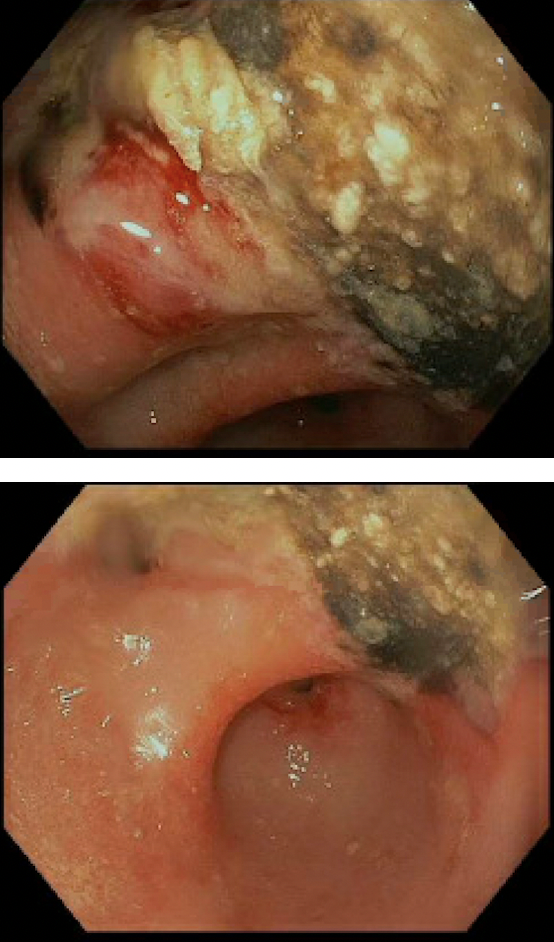
Esophagogastroduodenoscopy (EGD) revealed congested, erythematous and ulcerated mucosa in the gastric antrum. Biopsies demonstrated reactive gastropathy and purulent exudate with ample Actinomyces colonies and rare CMV viral inclusions. Of note, there was an undetectable serum CMV PCR during the same admit. The patient was discharged on IV Ampicillin (6 weeks) and oral Valganciclovir (21-day course). She then transitioned to oral amoxicillin for an additional 12 months. At 8-week follow-up endoscopy, a non- bleeding gastric ulcer was seen with biopsies indicating moderate active chronic gastritis and reactive epithelial changes, but without Actinomyces or CMV.
Discussion: Actinomycosis is difficult to diagnose by virtue of its rarity and indolent course. A palpable mass, sinus tract, or fistula may be present; but more uncommon gastrointestinal manifestations, such as gastric ulcerations, may be found. Radiographic imaging is non-specific, though CT may be useful localizing the extent of disease burden. Biopsy is the gold standard for diagnosis and should be pursued, especially in immunosuppressed patients.
Disclosures:
Mohammad T. Sultan, DO, MS, Luke Townsend, MD, Matthew Rice, MD. B0728 - An Unusual Culprit for Gastric Ulceration, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Ochsner Clinic Foundation, New Orleans, LA
Introduction: Actinomycosis is a chronic granulomatous disease caused by an anaerobic, gram positive, filamentous bacterium. Actinomycetes are commensal oral/intestinal bacteria that can manifest with fibrosis/necrosis, abscess formation, draining sinuses and fistulas when they invade susceptible tissue. Infection commonly affects the cervicofacial region (50%), however the literature describes abdominal involvement in 20% of cases (typically localized in the appendix and ileocecum). We describe a case of gastric ulceration secondary to actinomycosis.
Case Description/Methods: A 33-year-old female with Type 1 Diabetes Mellitus status post kidney-pancreas transplant on immunosuppression presents with one month of progressive, diffuse abdominal pain. Initial evaluation revealed acute renal failure of unclear etiology (creatinine of 5 from baseline of 1). Kidney biopsy revealed acute antibody mediated cellular rejection with donor specific antibodies. Methylprednisolone, PLEX and thymoglobulin were started. The patient’s ongoing rigors and abdominal pain prompted an infectious workup. Blood cultures returned with Group B Strep and Computed Tomography (CT) abdomen/pelvis without contrast showed diffuse gastric wall thickening and effacement of the gastric rugal folds.
Esophagogastroduodenoscopy (EGD) revealed congested, erythematous and ulcerated mucosa in the gastric antrum. Biopsies demonstrated reactive gastropathy and purulent exudate with ample Actinomyces colonies and rare CMV viral inclusions. Of note, there was an undetectable serum CMV PCR during the same admit. The patient was discharged on IV Ampicillin (6 weeks) and oral Valganciclovir (21-day course). She then transitioned to oral amoxicillin for an additional 12 months. At 8-week follow-up endoscopy, a non- bleeding gastric ulcer was seen with biopsies indicating moderate active chronic gastritis and reactive epithelial changes, but without Actinomyces or CMV.
Discussion: Actinomycosis is difficult to diagnose by virtue of its rarity and indolent course. A palpable mass, sinus tract, or fistula may be present; but more uncommon gastrointestinal manifestations, such as gastric ulcerations, may be found. Radiographic imaging is non-specific, though CT may be useful localizing the extent of disease burden. Biopsy is the gold standard for diagnosis and should be pursued, especially in immunosuppressed patients.
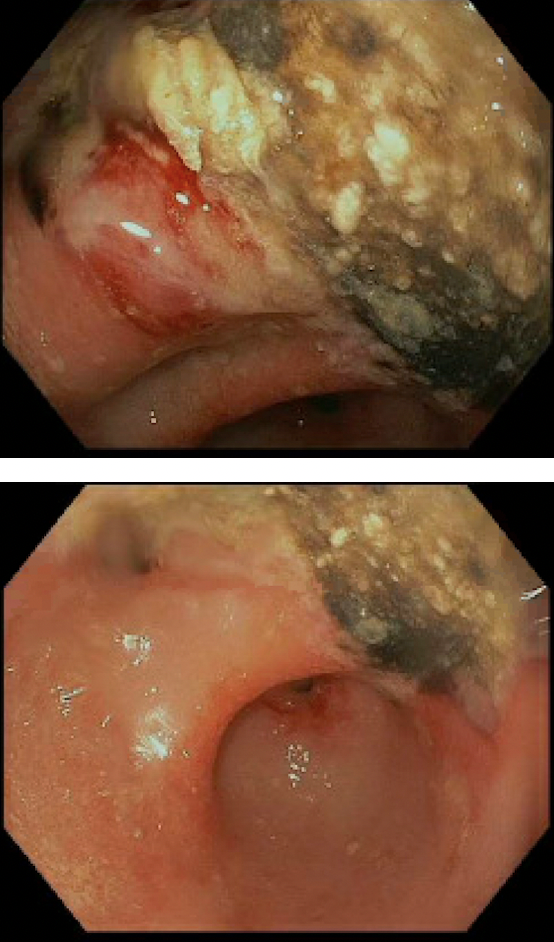
Figure: Figure 1: Images demonstrating severe mucosal changes characterized by congestion, erythema, granularity and ulceration at the incisura and gastric antrum. White nodular areas and signs of possible necrosis.
Disclosures:
Mohammad Sultan indicated no relevant financial relationships.
Luke Townsend indicated no relevant financial relationships.
Matthew Rice indicated no relevant financial relationships.
Mohammad T. Sultan, DO, MS, Luke Townsend, MD, Matthew Rice, MD. B0728 - An Unusual Culprit for Gastric Ulceration, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
