Back

Poster Session C - Monday Afternoon
Category: IBD
C0405 - Epidemiology of Documented Cannabis Use and/or Cannabis-Related Disorders in a Multi-Center Cohort of Inflammatory Bowel Disease Patients From 2012-2021
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio
- VN
Vu Q. Nguyen, MD
University Hospitals, Case Western Reserve University
Cleveland, OH
Presenting Author(s)
Vu Q. Nguyen, MD1, Jaime Abraham Perez, PhD2, Fabiano Celio, PhD3, Scott A. Martin, PhD4, Samuel Tanner, MD4, Jeffry Katz, MD1, Fabio Cominelli, MD, PhD1
1University Hospitals, Case Western Reserve University, Cleveland, OH; 2University Hospitals Clinical Research Center, Cleveland, OH; 3Case Western Reserve University, Cleveland, OH; 4University Hospitals Cleveland Medical Center, Cleveland, OH
Introduction: Cannabis has been used for medicinal or recreational purposes since ancient time. Prior studies have shown that cannabis may provide symptom relief in inflammatory bowel disease (IBD) patients. However, chronic cannabis use has also been associated with various gastrointestinal disorders such as cannabinoid hyperemesis syndrome. The aim of this study was to examine the epidemiology of cannabis use and/or cannabis-related disorders (CU-RD) in IBD versus non-IBD patients as documented in the electronic health records (EHR) of a large multi-center patient cohort.
Methods: We performed a retrospective cohort analysis examining the overall and annual incidence and prevalence rates of CU-RD in IBD versus non-IBD patients in TriNetX (Cambridge, MA), a multi-center research network comprising of EHR from 59 heath care organizations in the United States. Incident diagnoses of CU-RD from 1/1/2012 to 12/31/2021 were captured using ICD-10 codes F12.x for cannabis-related disorders or laboratory tests positive for the presence of cannabinoids or tetrahydrocannabinol. IBD was identified by ICD-10 codes K50 as Crohn’s disease (CD) or K51 as ulcerative colitis (UC). Chi-square tests were performed to compare categorical values and linear regression was used to analyze trends of continuous data.
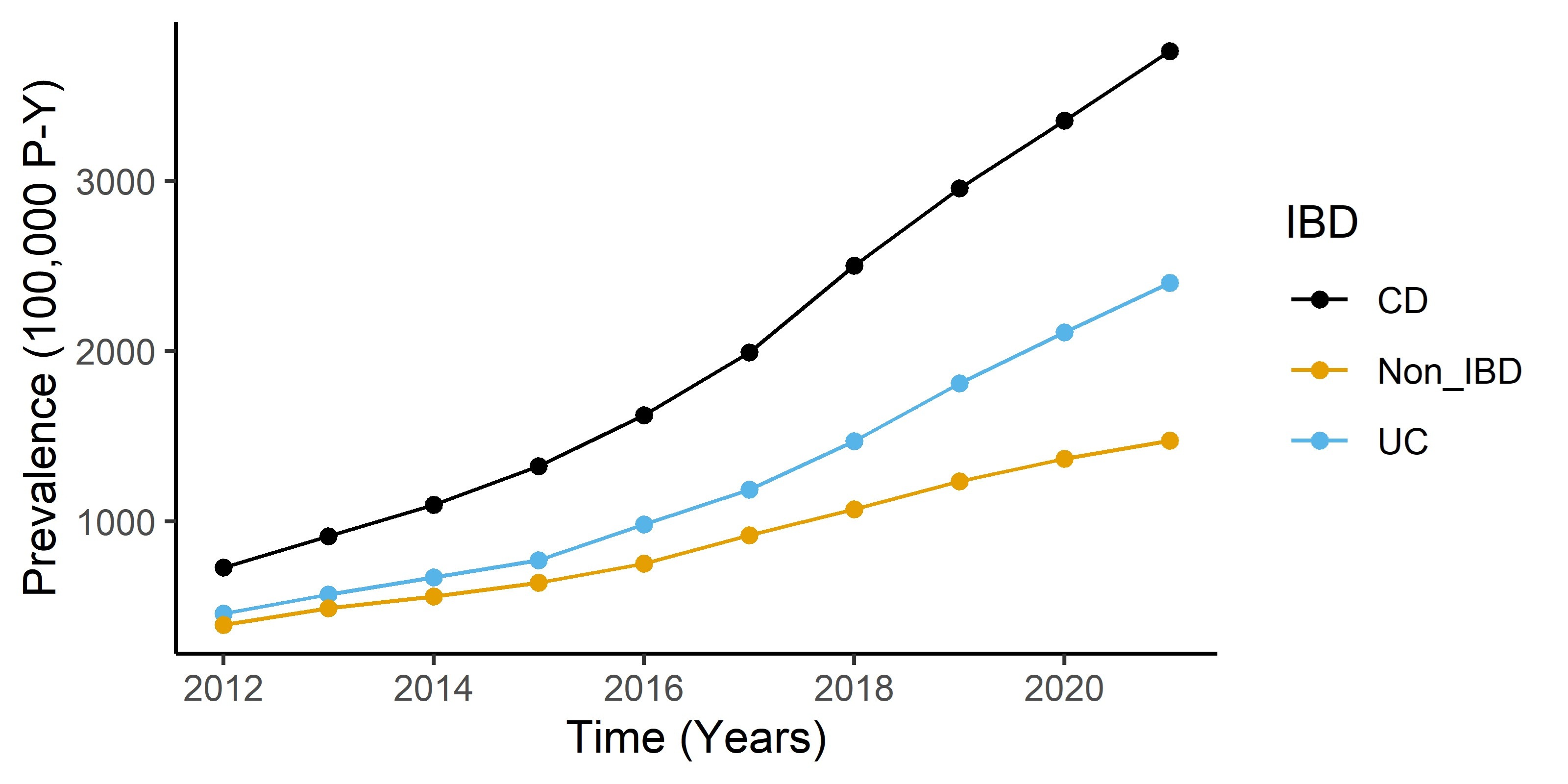
Results: From 2012 to 2021, the incidence rates of CU-RD in CD, UC, and non-IBD patients were 1.74, 1.03, and 0.98 per 100,000 persons respectively. There was a significantly higher prevalence of CU-RD in CD (3.43%, N=7,458) and UC (2.18%, N=4,413) compared to non-IBD patients (1.15%, N=791,430) [OR=3.06, CI: 2.99-3.14, and OR=1.81, CI: 1.75-1.86, respectively]. The prevalence of CU-RD in IBD and non-IBD patients has been rapidly rising over the past decade (Figure 1). CU-RD in IBD patients was more common in males compared to females (OR=1.44, CI: 1.39-1.49) and in African-Americans compared to other races (OR=2.56, CI: 2.45-2.68). CU-RD was most common in the young adult IBD population and was observed in disproportionately higher percentage in the Western states.
Discussion: The prevalence of CU-RD is rapidly rising in IBD patients. In a multi-center patient cohort, IBD patients have approximately 2 to 3 times higher odds of having CU-RD compared to non-IBD patients. More research is needed to examine the effect of cannabis in IBD.
Disclosures:
Vu Q. Nguyen, MD1, Jaime Abraham Perez, PhD2, Fabiano Celio, PhD3, Scott A. Martin, PhD4, Samuel Tanner, MD4, Jeffry Katz, MD1, Fabio Cominelli, MD, PhD1. C0405 - Epidemiology of Documented Cannabis Use and/or Cannabis-Related Disorders in a Multi-Center Cohort of Inflammatory Bowel Disease Patients From 2012-2021, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University Hospitals, Case Western Reserve University, Cleveland, OH; 2University Hospitals Clinical Research Center, Cleveland, OH; 3Case Western Reserve University, Cleveland, OH; 4University Hospitals Cleveland Medical Center, Cleveland, OH
Introduction: Cannabis has been used for medicinal or recreational purposes since ancient time. Prior studies have shown that cannabis may provide symptom relief in inflammatory bowel disease (IBD) patients. However, chronic cannabis use has also been associated with various gastrointestinal disorders such as cannabinoid hyperemesis syndrome. The aim of this study was to examine the epidemiology of cannabis use and/or cannabis-related disorders (CU-RD) in IBD versus non-IBD patients as documented in the electronic health records (EHR) of a large multi-center patient cohort.
Methods: We performed a retrospective cohort analysis examining the overall and annual incidence and prevalence rates of CU-RD in IBD versus non-IBD patients in TriNetX (Cambridge, MA), a multi-center research network comprising of EHR from 59 heath care organizations in the United States. Incident diagnoses of CU-RD from 1/1/2012 to 12/31/2021 were captured using ICD-10 codes F12.x for cannabis-related disorders or laboratory tests positive for the presence of cannabinoids or tetrahydrocannabinol. IBD was identified by ICD-10 codes K50 as Crohn’s disease (CD) or K51 as ulcerative colitis (UC). Chi-square tests were performed to compare categorical values and linear regression was used to analyze trends of continuous data.
Results: From 2012 to 2021, the incidence rates of CU-RD in CD, UC, and non-IBD patients were 1.74, 1.03, and 0.98 per 100,000 persons respectively. There was a significantly higher prevalence of CU-RD in CD (3.43%, N=7,458) and UC (2.18%, N=4,413) compared to non-IBD patients (1.15%, N=791,430) [OR=3.06, CI: 2.99-3.14, and OR=1.81, CI: 1.75-1.86, respectively]. The prevalence of CU-RD in IBD and non-IBD patients has been rapidly rising over the past decade (Figure 1). CU-RD in IBD patients was more common in males compared to females (OR=1.44, CI: 1.39-1.49) and in African-Americans compared to other races (OR=2.56, CI: 2.45-2.68). CU-RD was most common in the young adult IBD population and was observed in disproportionately higher percentage in the Western states.
Discussion: The prevalence of CU-RD is rapidly rising in IBD patients. In a multi-center patient cohort, IBD patients have approximately 2 to 3 times higher odds of having CU-RD compared to non-IBD patients. More research is needed to examine the effect of cannabis in IBD.
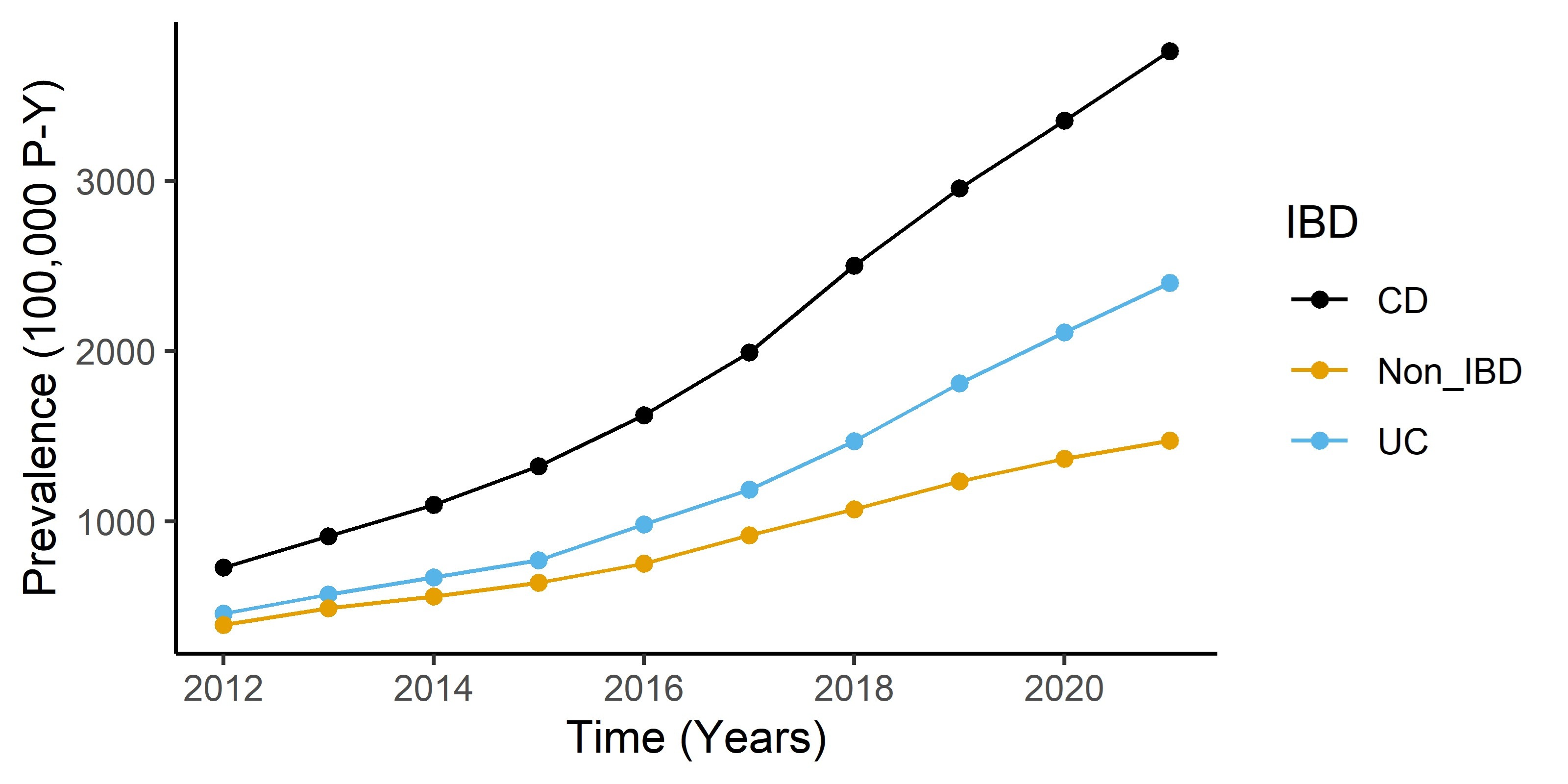
Figure: Figure 1: Prevalence of Cannabis Use and/or Cannabis-Related Disorders in IBD and non-IBD Patients in TriNetX from 2012-2021
Disclosures:
Vu Nguyen indicated no relevant financial relationships.
Jaime Abraham Perez indicated no relevant financial relationships.
Fabiano Celio indicated no relevant financial relationships.
Scott Martin indicated no relevant financial relationships.
Samuel Tanner indicated no relevant financial relationships.
Jeffry Katz indicated no relevant financial relationships.
Fabio Cominelli indicated no relevant financial relationships.
Vu Q. Nguyen, MD1, Jaime Abraham Perez, PhD2, Fabiano Celio, PhD3, Scott A. Martin, PhD4, Samuel Tanner, MD4, Jeffry Katz, MD1, Fabio Cominelli, MD, PhD1. C0405 - Epidemiology of Documented Cannabis Use and/or Cannabis-Related Disorders in a Multi-Center Cohort of Inflammatory Bowel Disease Patients From 2012-2021, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
