Back

Poster Session B - Monday Morning
Category: IBD
B0433 - Insulin-Like Growth Factor I Receptor Inhibitor-Induced Inflammatory Bowel Disease
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Julie Murone, DO
Allegheny Health Network
Pittsburgh, PA
Presenting Author(s)
Julie Murone, DO1, Evan Reinhart, DO2, Sandra El-Hachem, MD1
1Allegheny Health Network, Pittsburgh, PA; 2Allegheny General Hospital, Pittsburgh, PA
Introduction: Graves’ orbitopathy is an autoimmune disease that develops in approximately 40% of patients with Graves’ disease. Insulin-like growth factor I receptor (IGF-IR) is overexpressed in this disease and plays a central role in this ophthalmopathy. Teprotumumab is a monoclonal antibody against IGF-IR used for active Graves’ orbitopathy. We report a patient who presented with rectal bleeding and was found to have a reoccurrence of inflammatory bowel disease (IBD) thought to be secondary to recent teprotumumab therapy.
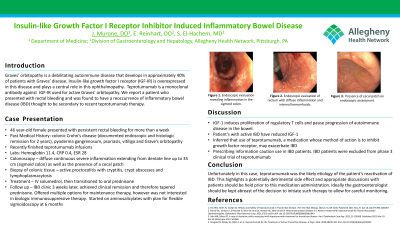
Case Description/Methods: A 46-year-old female with a diagnosis of Crohn’s disease, off of therapy for 4 years with endoscopic and histological remission, history of pyoderma gangrenosum, psoriasis, vitiligo, and Graves’ orbitopathy presented to the emergency department for rectal bleeding. On review, the patient had finished teprotumumab infusions 17 days prior to presentation. Following each infusion, she would experience 2 days of self-resolving rectal bleeding. After her last infusion, the bleeding persisted for more than a week leading her to seek medical care. Labs were significant for hemoglobin 11.4, CRP 0.4, and ESR 28. Colonoscopy revealed continuous severe inflammation extending from the dentate line up to the sigmoid colon as well as the presence of a cecal patch. Biopsies showed active proctocolitis with cryptitis, crypt abscesses and lymphoplasmacytosis. Patient was started on solumedrol 20 mg IV every 8 hours. Her symptoms resolved with the IV solumedrol and she was discharged home on a course of oral corticosteroids.
Discussion: IGF-1 induces proliferation of regulatory T cells and pauses progression of autoimmune disease in the bowel. Animal models have suggested that IGF-1 is involved in mucosal repair and has an anti-apoptotic function in gut mucosa. Patients with active IBD have reduced levels of IGF-1. Therefore, it could be inferred that the use of teprotumumab, a medication whose method of action is to inhibit this growth factor receptor, may exacerbate or illicit IBD. The drug prescribing information does caution that teprotumumab can trigger exacerbation of the underlying IBD and recommends close monitoring of IBD patients. This case highlights a potentially detrimental side effect and appropriate discussions with patients should be held prior to this medications usage. Ideally the gastroenterologist should be kept abreast of the decision to initiate such therapy to allow for careful monitoring.
Disclosures:
Julie Murone, DO1, Evan Reinhart, DO2, Sandra El-Hachem, MD1. B0433 - Insulin-Like Growth Factor I Receptor Inhibitor-Induced Inflammatory Bowel Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Allegheny Health Network, Pittsburgh, PA; 2Allegheny General Hospital, Pittsburgh, PA
Introduction: Graves’ orbitopathy is an autoimmune disease that develops in approximately 40% of patients with Graves’ disease. Insulin-like growth factor I receptor (IGF-IR) is overexpressed in this disease and plays a central role in this ophthalmopathy. Teprotumumab is a monoclonal antibody against IGF-IR used for active Graves’ orbitopathy. We report a patient who presented with rectal bleeding and was found to have a reoccurrence of inflammatory bowel disease (IBD) thought to be secondary to recent teprotumumab therapy.
Case Description/Methods: A 46-year-old female with a diagnosis of Crohn’s disease, off of therapy for 4 years with endoscopic and histological remission, history of pyoderma gangrenosum, psoriasis, vitiligo, and Graves’ orbitopathy presented to the emergency department for rectal bleeding. On review, the patient had finished teprotumumab infusions 17 days prior to presentation. Following each infusion, she would experience 2 days of self-resolving rectal bleeding. After her last infusion, the bleeding persisted for more than a week leading her to seek medical care. Labs were significant for hemoglobin 11.4, CRP 0.4, and ESR 28. Colonoscopy revealed continuous severe inflammation extending from the dentate line up to the sigmoid colon as well as the presence of a cecal patch. Biopsies showed active proctocolitis with cryptitis, crypt abscesses and lymphoplasmacytosis. Patient was started on solumedrol 20 mg IV every 8 hours. Her symptoms resolved with the IV solumedrol and she was discharged home on a course of oral corticosteroids.
Discussion: IGF-1 induces proliferation of regulatory T cells and pauses progression of autoimmune disease in the bowel. Animal models have suggested that IGF-1 is involved in mucosal repair and has an anti-apoptotic function in gut mucosa. Patients with active IBD have reduced levels of IGF-1. Therefore, it could be inferred that the use of teprotumumab, a medication whose method of action is to inhibit this growth factor receptor, may exacerbate or illicit IBD. The drug prescribing information does caution that teprotumumab can trigger exacerbation of the underlying IBD and recommends close monitoring of IBD patients. This case highlights a potentially detrimental side effect and appropriate discussions with patients should be held prior to this medications usage. Ideally the gastroenterologist should be kept abreast of the decision to initiate such therapy to allow for careful monitoring.
Disclosures:
Julie Murone indicated no relevant financial relationships.
Evan Reinhart indicated no relevant financial relationships.
Sandra El-Hachem: Abbvie – Advisory Committee/Board Member, Speakers Bureau. Bristol Myers Squibb – Speakers Bureau. Ferring – Speakers Bureau. Janssen – Speakers Bureau. Pfizer – Speakers Bureau. Prometheus – Advisory Committee/Board Member. Takeda – Speakers Bureau.
Julie Murone, DO1, Evan Reinhart, DO2, Sandra El-Hachem, MD1. B0433 - Insulin-Like Growth Factor I Receptor Inhibitor-Induced Inflammatory Bowel Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
