Back

Poster Session A - Sunday Afternoon
Category: IBD
A0398 - Twist and Shout: A Case Report of Twisted Pouch Syndrome
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Mathoula Bilalis, MD
LSUHSC
New Orleans, LA
Presenting Author(s)
Mathoula Bilalis, MD1, Lilia Stefaniwsky, MD1, Xena Zheng, BA1, Stephanie Eschete, PA-C1, Nisha Loganantharaj, MD2
1LSUHSC, New Orleans, LA; 2University Medical Center - LSUHSC, New Orleans, LA
Introduction: Total proctocolectomy (TPC) with ileal pouch-anal anastomosis (IPAA) is recommended in the setting of medically refractory ulcerative colitis (UC). Following reanastomosis, complications can occur. We present a case of a patient who developed recurrent obstructive symptoms four years after IPAA. Imaging was concerning for a stricture in the pre-pouch ileum although no stricture was noted on pouchoscopy. Twisted pouch syndrome (TPS) was suspected.
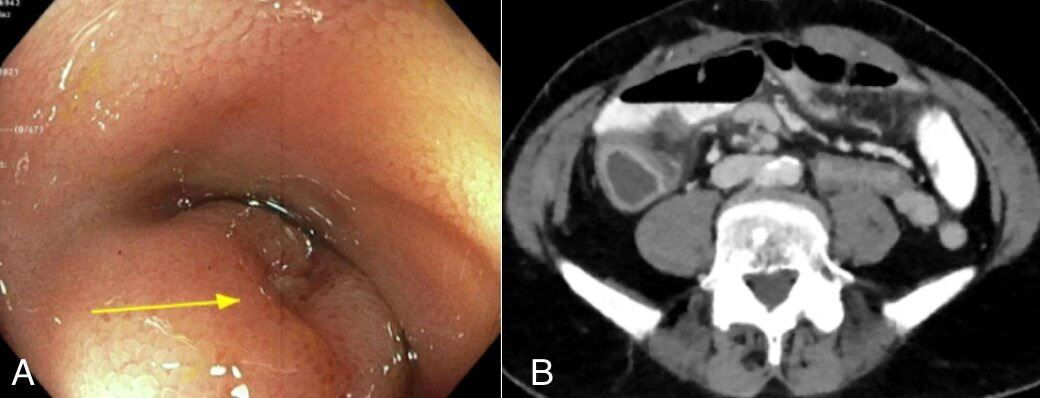
Case Description/Methods: A 61-year-old male with refractory UC status post TPC with IPAA presented to clinic for acute nausea, constipation, and epigastric pressure. CTE revealed a distended stomach and small bowel with multiple air-fluid levels as well as narrowing and a transition point at the anastomosis and in the more proximal ileum. Endoscopy revealed few aphthous ulcers in distal pre-pouch ileum; the anastomosis was easily traversed and no stricture was found. Eight months later, the patient presented for 4 weeks of severe, worsening, diffuse abdominal pain associated with alternating diarrhea and constipation, decreased oral intake, nausea, and vomiting. CT re-demonstrated potential stricture proximal to pouch with dilation of the distal ileum and scattered areas of distal small bowel thickening. Pouchoscopy showed few patchy aphthous ulcers in the pre-pouch ileum with dilation, an angulated pouch inlet, and a large aphthous ulcer following the pouch inlet that caused narrowing but no stricture. He was ultimately diagnosed with TPS.
Discussion: TPS is caused by intraoperative misalignment of the ileal pouch and manifests as erratic bowel habits, unexplained abdominal or pelvic pain, and obstructive symptoms. Although malrotated and twisted pouches are known complications of IPAA, TPS was only recently named to describe this triad of symptoms that has proven difficult to diagnose pre-operatively. A retrospective review of Cleveland Clinic’s Pouch Center registry of redo IPAA operative reports identified 29 cases of TPS with less than 25% of them diagnosed pre-operatively despite a thorough workup. Most cases were diagnosed intra-operatively and treated with redo surgery. This case is consistent with TPS, and the pouch ulceration and pouchitis seen could be due to mechanical stress and vascular insufficiency secondary to the twisting. More literature and awareness of TPS is needed to aid in proper diagnosis and management of these patients.
Disclosures:
Mathoula Bilalis, MD1, Lilia Stefaniwsky, MD1, Xena Zheng, BA1, Stephanie Eschete, PA-C1, Nisha Loganantharaj, MD2. A0398 - Twist and Shout: A Case Report of Twisted Pouch Syndrome, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1LSUHSC, New Orleans, LA; 2University Medical Center - LSUHSC, New Orleans, LA
Introduction: Total proctocolectomy (TPC) with ileal pouch-anal anastomosis (IPAA) is recommended in the setting of medically refractory ulcerative colitis (UC). Following reanastomosis, complications can occur. We present a case of a patient who developed recurrent obstructive symptoms four years after IPAA. Imaging was concerning for a stricture in the pre-pouch ileum although no stricture was noted on pouchoscopy. Twisted pouch syndrome (TPS) was suspected.
Case Description/Methods: A 61-year-old male with refractory UC status post TPC with IPAA presented to clinic for acute nausea, constipation, and epigastric pressure. CTE revealed a distended stomach and small bowel with multiple air-fluid levels as well as narrowing and a transition point at the anastomosis and in the more proximal ileum. Endoscopy revealed few aphthous ulcers in distal pre-pouch ileum; the anastomosis was easily traversed and no stricture was found. Eight months later, the patient presented for 4 weeks of severe, worsening, diffuse abdominal pain associated with alternating diarrhea and constipation, decreased oral intake, nausea, and vomiting. CT re-demonstrated potential stricture proximal to pouch with dilation of the distal ileum and scattered areas of distal small bowel thickening. Pouchoscopy showed few patchy aphthous ulcers in the pre-pouch ileum with dilation, an angulated pouch inlet, and a large aphthous ulcer following the pouch inlet that caused narrowing but no stricture. He was ultimately diagnosed with TPS.
Discussion: TPS is caused by intraoperative misalignment of the ileal pouch and manifests as erratic bowel habits, unexplained abdominal or pelvic pain, and obstructive symptoms. Although malrotated and twisted pouches are known complications of IPAA, TPS was only recently named to describe this triad of symptoms that has proven difficult to diagnose pre-operatively. A retrospective review of Cleveland Clinic’s Pouch Center registry of redo IPAA operative reports identified 29 cases of TPS with less than 25% of them diagnosed pre-operatively despite a thorough workup. Most cases were diagnosed intra-operatively and treated with redo surgery. This case is consistent with TPS, and the pouch ulceration and pouchitis seen could be due to mechanical stress and vascular insufficiency secondary to the twisting. More literature and awareness of TPS is needed to aid in proper diagnosis and management of these patients.
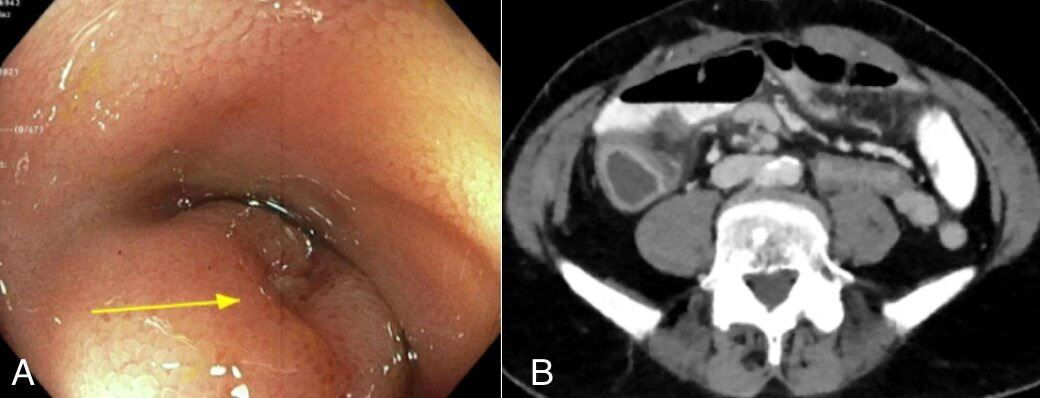
Figure: A: Narrowing caused by large ulcer in pre-pouch ileum
B: Dilated distal ileum with wall thickening and segment of luminal narrowing proximal to pouch
B: Dilated distal ileum with wall thickening and segment of luminal narrowing proximal to pouch
Disclosures:
Mathoula Bilalis indicated no relevant financial relationships.
Lilia Stefaniwsky indicated no relevant financial relationships.
Xena Zheng indicated no relevant financial relationships.
Stephanie Eschete indicated no relevant financial relationships.
Nisha Loganantharaj: Abbvie – Speakers Bureau.
Mathoula Bilalis, MD1, Lilia Stefaniwsky, MD1, Xena Zheng, BA1, Stephanie Eschete, PA-C1, Nisha Loganantharaj, MD2. A0398 - Twist and Shout: A Case Report of Twisted Pouch Syndrome, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
