Back

Poster Session B - Monday Morning
Category: Liver
B0579 - Pregnancy-Induced Type 2 Autoimmune Hepatitis
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Brandon H. Busch, MD
University of Louisville
Louisville, KY
Presenting Author(s)
Brandon H. Busch, MD, Michael Eiswerth, DO, Freeha Khan, MD, Matthew Cave, MD
University of Louisville, Louisville, KY
Introduction: Pregnancy has been established as a risk factor for the generation of autoimmune disease. The pathophysiology linking pregnancy and autoimmune disease is not well-established but hypothesized to be a result of hormonal modulation and fetal microchimerism. We report a case of Type 2 Autoimmune Hepatitis (AIH) that is elicited by pregnancy as confirmed by the presence of high titer anti-LKM (Liver-Kidney Microsomal) antibodies and classic histopathologic findings. To our knowledge, this is the first reported case of Type 2 Autoimmune Hepatitis directly triggered by pregnancy.
Case Description/Methods: A 19-year-old female with a history of recent uncomplicated pregnancy with successful delivery 3 months prior presented to the hospital with complaint of 1 week of right upper quadrant pain and 2 days of itching and yellowing of her skin. Exam showed scleral icterus and jaundice while abdomen was negative for tenderness or palpable mass. Labs revealed elevated AST at 670 U/L, ALT of 1107, ALP of 329 U/L, total bilirubin of 6.7 mg/dL, conjugated bilirubin of 4.8 mg/dL, unconjugated bilirubin of 1.9 mg/dL, and an INR of 1.3. These labs were all within normal limits 3 months prior to admission. Further workup revealed positive anti-liver-kidney (anti-LKM) antibodies with a titer of >1:2560. Imaging was normal. Liver biopsy revealed interface hepatitis, plasma cell infiltration, apoptotic hepatocytes, emperipolesis and rosette formation consistent with autoimmune hepatitis.
Discussion: The mechanism for initiation of autoimmune disease is of great interest and is unclear in the setting of pregnancy. It has been hypothesized that exchange of fetal and maternal cells occurs, known as fetal microchimerism, which may be a trigger for generation of autoimmune disease in pregnancy. This mechanism is proposed to be through immune sensitization by exposure to HLA-susceptibility alleles or through a graft-vs-host type of mechanism. Another proposed mechanism suggests that hormonal fluctuations mediate a shift between Th1 and Th2-mediated immunity during pregnancy. In the 3rd trimester and continuing into the postpartum period, there is a decrease in hCG which results in decreased expression of T-regulatory populations and resultant increase in inflammation. Prolactin increases which results in increased production of proinflammatory TNF-α, INF-γ, and IL-2. We believe this patient had a defect in allogeneic immune tolerance during pregnancy with resultant initial flare of AIH in the post-partum period.
Disclosures:
Brandon H. Busch, MD, Michael Eiswerth, DO, Freeha Khan, MD, Matthew Cave, MD. B0579 - Pregnancy-Induced Type 2 Autoimmune Hepatitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
University of Louisville, Louisville, KY
Introduction: Pregnancy has been established as a risk factor for the generation of autoimmune disease. The pathophysiology linking pregnancy and autoimmune disease is not well-established but hypothesized to be a result of hormonal modulation and fetal microchimerism. We report a case of Type 2 Autoimmune Hepatitis (AIH) that is elicited by pregnancy as confirmed by the presence of high titer anti-LKM (Liver-Kidney Microsomal) antibodies and classic histopathologic findings. To our knowledge, this is the first reported case of Type 2 Autoimmune Hepatitis directly triggered by pregnancy.
Case Description/Methods: A 19-year-old female with a history of recent uncomplicated pregnancy with successful delivery 3 months prior presented to the hospital with complaint of 1 week of right upper quadrant pain and 2 days of itching and yellowing of her skin. Exam showed scleral icterus and jaundice while abdomen was negative for tenderness or palpable mass. Labs revealed elevated AST at 670 U/L, ALT of 1107, ALP of 329 U/L, total bilirubin of 6.7 mg/dL, conjugated bilirubin of 4.8 mg/dL, unconjugated bilirubin of 1.9 mg/dL, and an INR of 1.3. These labs were all within normal limits 3 months prior to admission. Further workup revealed positive anti-liver-kidney (anti-LKM) antibodies with a titer of >1:2560. Imaging was normal. Liver biopsy revealed interface hepatitis, plasma cell infiltration, apoptotic hepatocytes, emperipolesis and rosette formation consistent with autoimmune hepatitis.
Discussion: The mechanism for initiation of autoimmune disease is of great interest and is unclear in the setting of pregnancy. It has been hypothesized that exchange of fetal and maternal cells occurs, known as fetal microchimerism, which may be a trigger for generation of autoimmune disease in pregnancy. This mechanism is proposed to be through immune sensitization by exposure to HLA-susceptibility alleles or through a graft-vs-host type of mechanism. Another proposed mechanism suggests that hormonal fluctuations mediate a shift between Th1 and Th2-mediated immunity during pregnancy. In the 3rd trimester and continuing into the postpartum period, there is a decrease in hCG which results in decreased expression of T-regulatory populations and resultant increase in inflammation. Prolactin increases which results in increased production of proinflammatory TNF-α, INF-γ, and IL-2. We believe this patient had a defect in allogeneic immune tolerance during pregnancy with resultant initial flare of AIH in the post-partum period.
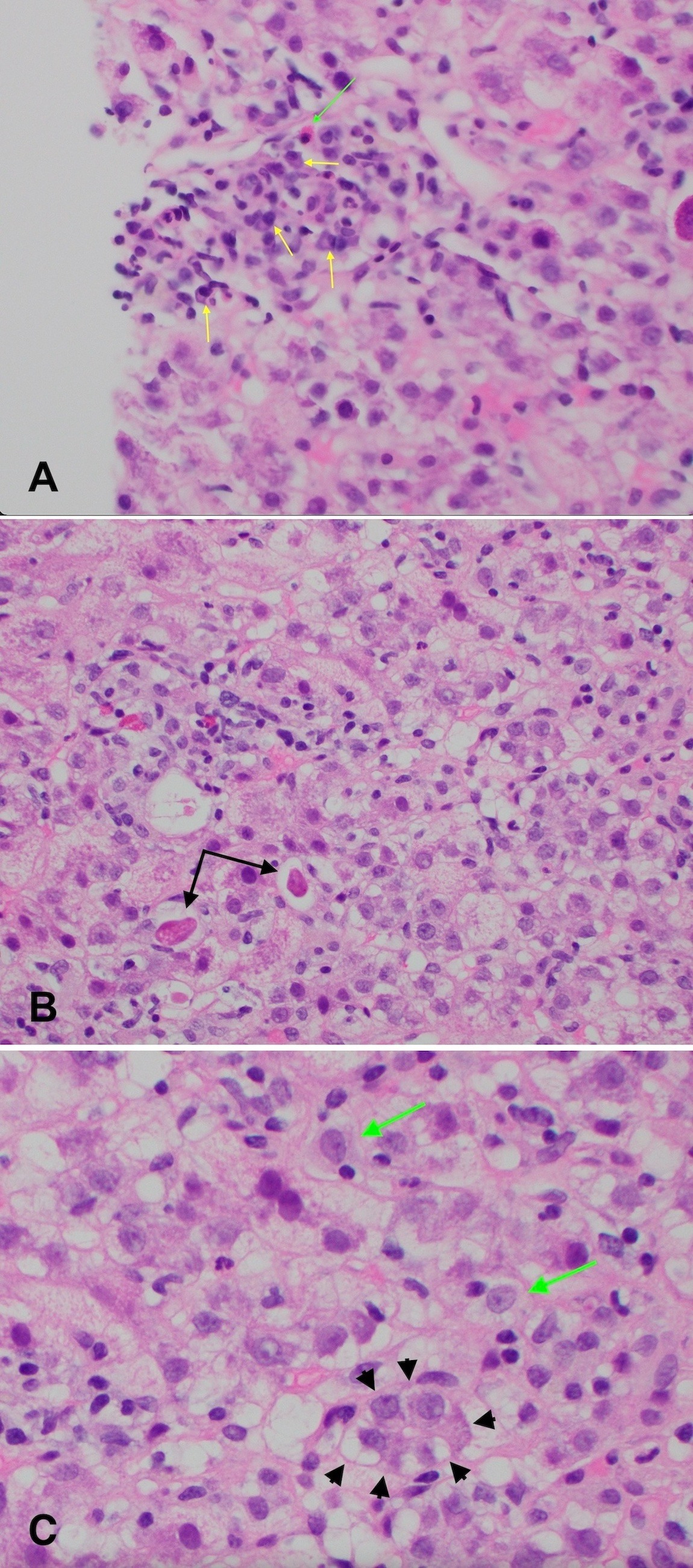
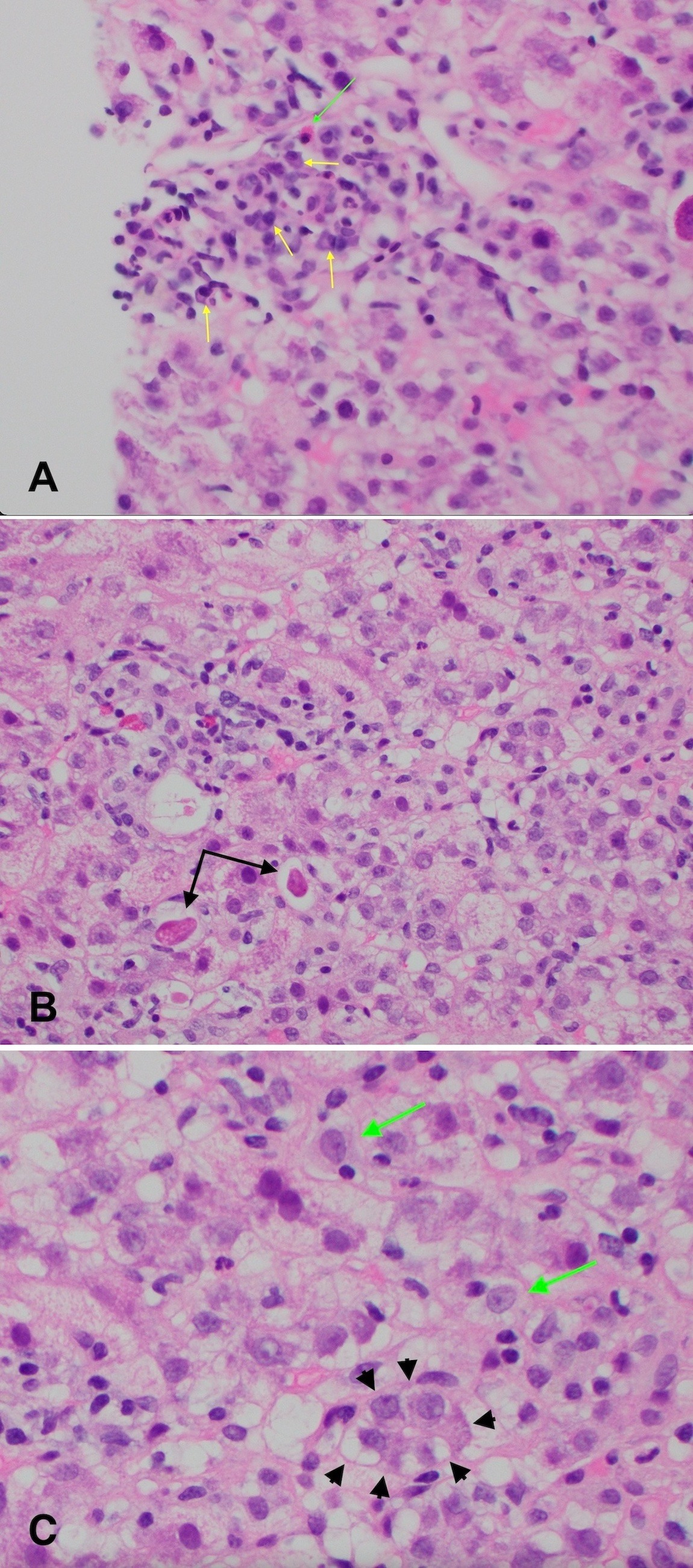
Figure: Figure 1A: H&E stain at 400x magnification. Portal tract with lymphocytic infiltrate into surrounding hepatocytes consistent with interface hepatitis. Plasma cells present and indicated by yellow arrows. A lone eosinophil indicated by the green arrow.
Figure 1B: H&E stain at 400x magnification. Acidophil bodies present (indicated by black arrows) which represent apoptotic hepatocytes, found in a background of lobular inflammation.
Figure 1C: H&E stain at 400x magnification. Emperipolesis is present (indicated by green arrows) and is characterized by infiltration of lymphocytes into the cytoplasm of a hepatocyte. Rosette formation observed (outlined by black arrowheads) which represents small groups of hepatocytes arranged around a lumen and thought to be indicative of hepatocellular regeneration. Emperipolesis and rosette formation are thought to be typical of autoimmune hepatitis.
Figure 1B: H&E stain at 400x magnification. Acidophil bodies present (indicated by black arrows) which represent apoptotic hepatocytes, found in a background of lobular inflammation.
Figure 1C: H&E stain at 400x magnification. Emperipolesis is present (indicated by green arrows) and is characterized by infiltration of lymphocytes into the cytoplasm of a hepatocyte. Rosette formation observed (outlined by black arrowheads) which represents small groups of hepatocytes arranged around a lumen and thought to be indicative of hepatocellular regeneration. Emperipolesis and rosette formation are thought to be typical of autoimmune hepatitis.
Disclosures:
Brandon Busch indicated no relevant financial relationships.
Michael Eiswerth indicated no relevant financial relationships.
Freeha Khan indicated no relevant financial relationships.
Matthew Cave indicated no relevant financial relationships.
Brandon H. Busch, MD, Michael Eiswerth, DO, Freeha Khan, MD, Matthew Cave, MD. B0579 - Pregnancy-Induced Type 2 Autoimmune Hepatitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
