Back

Poster Session B - Monday Morning
Category: Stomach
B0724 - Common Variable Immunodeficiency and Gastric Carcinogenesis: Two Illustrative Cases
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Drew Levy, BS
Texas A&M Intercollegiate School of Engineering Medicine
Houston, TX
Presenting Author(s)
Drew Levy, BS1, Mary R. Schwartz, MD2, Zunirah Ahmed, MD2, Sunil Dacha, MD2, Nestor F. Esnaola, MD, MPH2, Eamonn M. Quigley, MD, MACG2
1Texas A&M Intercollegiate School of Engineering Medicine, Houston, TX; 2Houston Methodist Hospital, Houston, TX
Introduction: Common variable immunodeficiency (CVID) is linked to an increased risk for gastric cancer which seems to be associated with achlorhydria, H. pylori infection, decreased production of gastric IgA, and autoimmune phenomena. We present two patients illustrating progression of gastric pathology in CVID through dysplasia to cancer.
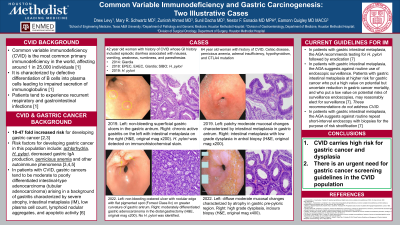
Case Description/Methods: A 42-year-old woman with CVID presented with dyspepsia, diarrhea and a 75 lb weight loss. Small intestinal bacterial overgrowth was diagnosed and treated. EGD revealed a superficial ulcer at the incisura. Pathological examination demonstrated chronic active gastritis with H. pylori and intestinal metaplasia (IM) without dysplasia. Triple therapy was unsuccessful; repeat EGD 1 year later demonstrated 3 superficial ulcers at the incisura and antrum; biopsies revealed chronic active gastritis with H. pylori and IM without dysplasia. Second-line therapy failed. 3 years later, EGD showed a non-bleeding cratered ulcer with a nodular edge on the greater curvature in the antrum. Biopsies demonstrated an invasive tubular adenocarcinoma arising in a background of IM with low and high grade dysplasia and no evidence of H. pylori. Partial gastrectomy with Roux-en-Y gastrojejunostomy and modified D2 lymphadenectomy was performed. Pathologic examination confirmed a T1aN0M0 moderately differentiated adenocarcinoma.
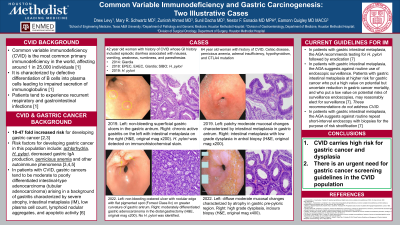
A 64-year-old woman with CVID, celiac disease, pernicious anemia and a CTLA4 gene mutation presented in 2019 for surveillance following removal of a gastric adenoma by EMR 2 months earlier. From 2018-2022, EGDs with gastric mapping were performed every 6 months and revealed progression from low to focal high grade dysplasia. In 2019, surveillance biopsies showed foci of low and high grade dysplasia in the antrum. EMR of a sessile polyp and ESD of 2 sessile polyps were performed followed by EMR of a sessile antral polyp and EMR of diffusely nodular mucosa at the incisura 5 months later. Biopsies have been consistently negative for H. pylori.
Discussion: These cases illustrate progression to cancer in CVID and exemplify two risk factors: Helicobacter pylori and achlorhydria. Both progressed from low to high grade dysplasia and, in one, to invasive cancer within 4 years. Guidance on surveillance for IM in the non-CVID population varies in terms of frequency and intervals; with the risk of progression to cancer in CVID increased 10-47-fold, there is an urgent need for guidelines on surveillance.
Disclosures:
Drew Levy, BS1, Mary R. Schwartz, MD2, Zunirah Ahmed, MD2, Sunil Dacha, MD2, Nestor F. Esnaola, MD, MPH2, Eamonn M. Quigley, MD, MACG2. B0724 - Common Variable Immunodeficiency and Gastric Carcinogenesis: Two Illustrative Cases, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Texas A&M Intercollegiate School of Engineering Medicine, Houston, TX; 2Houston Methodist Hospital, Houston, TX
Introduction: Common variable immunodeficiency (CVID) is linked to an increased risk for gastric cancer which seems to be associated with achlorhydria, H. pylori infection, decreased production of gastric IgA, and autoimmune phenomena. We present two patients illustrating progression of gastric pathology in CVID through dysplasia to cancer.
Case Description/Methods: A 42-year-old woman with CVID presented with dyspepsia, diarrhea and a 75 lb weight loss. Small intestinal bacterial overgrowth was diagnosed and treated. EGD revealed a superficial ulcer at the incisura. Pathological examination demonstrated chronic active gastritis with H. pylori and intestinal metaplasia (IM) without dysplasia. Triple therapy was unsuccessful; repeat EGD 1 year later demonstrated 3 superficial ulcers at the incisura and antrum; biopsies revealed chronic active gastritis with H. pylori and IM without dysplasia. Second-line therapy failed. 3 years later, EGD showed a non-bleeding cratered ulcer with a nodular edge on the greater curvature in the antrum. Biopsies demonstrated an invasive tubular adenocarcinoma arising in a background of IM with low and high grade dysplasia and no evidence of H. pylori. Partial gastrectomy with Roux-en-Y gastrojejunostomy and modified D2 lymphadenectomy was performed. Pathologic examination confirmed a T1aN0M0 moderately differentiated adenocarcinoma.
A 64-year-old woman with CVID, celiac disease, pernicious anemia and a CTLA4 gene mutation presented in 2019 for surveillance following removal of a gastric adenoma by EMR 2 months earlier. From 2018-2022, EGDs with gastric mapping were performed every 6 months and revealed progression from low to focal high grade dysplasia. In 2019, surveillance biopsies showed foci of low and high grade dysplasia in the antrum. EMR of a sessile polyp and ESD of 2 sessile polyps were performed followed by EMR of a sessile antral polyp and EMR of diffusely nodular mucosa at the incisura 5 months later. Biopsies have been consistently negative for H. pylori.
Discussion: These cases illustrate progression to cancer in CVID and exemplify two risk factors: Helicobacter pylori and achlorhydria. Both progressed from low to high grade dysplasia and, in one, to invasive cancer within 4 years. Guidance on surveillance for IM in the non-CVID population varies in terms of frequency and intervals; with the risk of progression to cancer in CVID increased 10-47-fold, there is an urgent need for guidelines on surveillance.
Disclosures:
Drew Levy indicated no relevant financial relationships.
Mary Schwartz indicated no relevant financial relationships.
Zunirah Ahmed indicated no relevant financial relationships.
Sunil Dacha indicated no relevant financial relationships.
Nestor Esnaola indicated no relevant financial relationships.
Eamonn Quigley: Biomerica – Grant/Research Support. Vibrant – Advisor or Review Panel Member. Vibrant – Clinical Advisory Board.
Drew Levy, BS1, Mary R. Schwartz, MD2, Zunirah Ahmed, MD2, Sunil Dacha, MD2, Nestor F. Esnaola, MD, MPH2, Eamonn M. Quigley, MD, MACG2. B0724 - Common Variable Immunodeficiency and Gastric Carcinogenesis: Two Illustrative Cases, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
