Back

Poster Session B - Monday Morning
Category: Liver
B0610 - COVID-19 Vaccination May Increase the Risk of Autoimmune Hepatitis in Patients With Underlying Autoimmune Disease
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Omar Saab, MBChB
NewYork Presbyterian Queens Hospital
Flushing, NY
Presenting Author(s)
Omar Saab, MBChB1, Marwah Algodi, MBChB2, Ahmed Gemei, MD1, Syed Hussain, MD1
1NewYork Presbyterian Queens Hospital, Flushing, NY; 2Ibn Al Nafees Hospital, Flushing, NY
Introduction: It is established that COVID-19 viral infection is associated with many autoimmune processes, especially in predisposed patients, such as autoimmune hepatitis AIH [1,2]. Molecular mimicry is one of the suggested mechanisms behind such phenomena. mRNA COVID-19 vaccination can plays the same role as the infection does.
Case Description/Methods: 55 year old Hispanic male with ulcerative colitis on home sulfasalazine who presented to the ED with complaints of a vague, non-cramping, and dull RUQ abdominal pain for 3 weeks duration. Negative ROS.
The patient’s social history is unremarkable. No recent travel, occupational exposures, herbal supplements use, or acetaminophen use.
He received 2 doses of Pfizer COVID -19 vaccines , last dose was around 21 days before admission.
VS were normal, physical examination was remarkable for jaundice and mild RUQ tenderness.
laboratory tests were remarkable for: Liver Function Tests: AST/ALT 1621/1476 units per liter (U/L) , T. bilirubin 6.0 milligrams per deciliter (mg/dL), D.bilirubin 4.5 (mg/dL), Alkaline phosphatase 167 (U/L) , GGT: 339 , ESR: 99 mm, CRP: 3.40 (mg/dL).
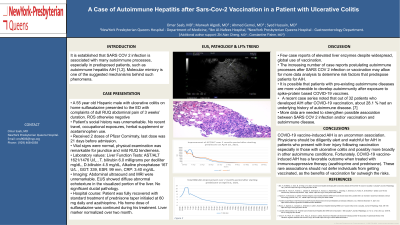
Abdominal ultrasound and MRI were unremarkable. EUS showed a diffuse abnormal echotexture in the visualized portion of the liver. No significant ductal pathology.
The patient was treated with azathioprine and prednisone 60 mg daily with slow tapering and with continuation of his home dose sulfasalazine.
Discussion: Few case reports were reported over billions of doses of vaccine administration.
The increasing number of case reports associating autoimmune processes with COVID-19 related infection and mRNA vaccines might allow for more data analysis to determine risk factors that predispose patients for AIH.
It is likely that patients with pre-existing autoimmune diseases are more vulnerable to develop autoimmunity after exposure to spike-protein based COVID-19 vaccines.
If more data confirms causality of COVID-19 vaccine induced AIH, this will help providers to identify patient at high risk to develop AIH as a side effect, and also may encourage scientists to find out other types of vaccines that has low/no chance of molecular mimicry.

Disclosures:
Omar Saab, MBChB1, Marwah Algodi, MBChB2, Ahmed Gemei, MD1, Syed Hussain, MD1. B0610 - COVID-19 Vaccination May Increase the Risk of Autoimmune Hepatitis in Patients With Underlying Autoimmune Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1NewYork Presbyterian Queens Hospital, Flushing, NY; 2Ibn Al Nafees Hospital, Flushing, NY
Introduction: It is established that COVID-19 viral infection is associated with many autoimmune processes, especially in predisposed patients, such as autoimmune hepatitis AIH [1,2]. Molecular mimicry is one of the suggested mechanisms behind such phenomena. mRNA COVID-19 vaccination can plays the same role as the infection does.
Case Description/Methods: 55 year old Hispanic male with ulcerative colitis on home sulfasalazine who presented to the ED with complaints of a vague, non-cramping, and dull RUQ abdominal pain for 3 weeks duration. Negative ROS.
The patient’s social history is unremarkable. No recent travel, occupational exposures, herbal supplements use, or acetaminophen use.
He received 2 doses of Pfizer COVID -19 vaccines , last dose was around 21 days before admission.
VS were normal, physical examination was remarkable for jaundice and mild RUQ tenderness.
laboratory tests were remarkable for: Liver Function Tests: AST/ALT 1621/1476 units per liter (U/L) , T. bilirubin 6.0 milligrams per deciliter (mg/dL), D.bilirubin 4.5 (mg/dL), Alkaline phosphatase 167 (U/L) , GGT: 339 , ESR: 99 mm, CRP: 3.40 (mg/dL).
Abdominal ultrasound and MRI were unremarkable. EUS showed a diffuse abnormal echotexture in the visualized portion of the liver. No significant ductal pathology.
The patient was treated with azathioprine and prednisone 60 mg daily with slow tapering and with continuation of his home dose sulfasalazine.
Discussion: Few case reports were reported over billions of doses of vaccine administration.
The increasing number of case reports associating autoimmune processes with COVID-19 related infection and mRNA vaccines might allow for more data analysis to determine risk factors that predispose patients for AIH.
It is likely that patients with pre-existing autoimmune diseases are more vulnerable to develop autoimmunity after exposure to spike-protein based COVID-19 vaccines.
If more data confirms causality of COVID-19 vaccine induced AIH, this will help providers to identify patient at high risk to develop AIH as a side effect, and also may encourage scientists to find out other types of vaccines that has low/no chance of molecular mimicry.

Figure: Liver biopsy - histopathology
Disclosures:
Omar Saab indicated no relevant financial relationships.
Marwah Algodi indicated no relevant financial relationships.
Ahmed Gemei indicated no relevant financial relationships.
Syed Hussain indicated no relevant financial relationships.
Omar Saab, MBChB1, Marwah Algodi, MBChB2, Ahmed Gemei, MD1, Syed Hussain, MD1. B0610 - COVID-19 Vaccination May Increase the Risk of Autoimmune Hepatitis in Patients With Underlying Autoimmune Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
