Back

Poster Session B - Monday Morning
Category: Liver
B0564 - Acute Alcoholic Hepatitis With Portal Hypertension Complicated by Tuberculous Peritonitis and Ascites
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Katya Swarts, MD
University of Virginia Health System
Charlottesville, VA
Presenting Author(s)
Award: Presidential Poster Award
Katya Swarts, MD1, Leland Stratton, MD2, Anuragh R. Gudur, MD1, Stephen Caldwell, MD2
1University of Virginia Health System, Charlottesville, VA; 2University of Virginia, Charlottesville, VA
Introduction: Peritonitis related to tuberculosis (TB) infection is rare in the US and normally associated with immunocompromised states. We present a patient found to have TB peritonitis during evaluation of alcoholic hepatitis without evident lung disease.
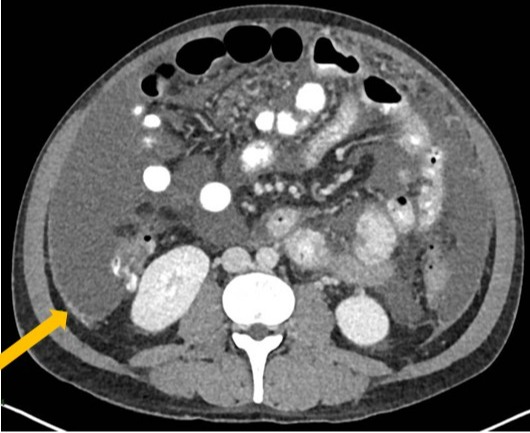
Case Description/Methods: The patient is a 39 yo male born in Mexico with no medical history who presented with three days of abdominal distention, jaundice, and fevers in the setting of alcohol use disorder. He had no other historic risk factors for TB or cough. Exam was remarkable for a distended abdomen. Laboratory results showed leukocytosis, total bilirubin 3.5 (mg/dL), alkaline phosphatase 295 (U/L), AST 147 (U/L), ALT 62 (U/L), and positive quantiferon gold. Chest x-ray had no pulmonary lesions. Ascites fluid studies were significant for high white count (2214 k/uL) with lymphocytic predominance (91%). The serum ascites albumin gradient was consistent with portal hypertension, and ascites total protein was elevated (3.6 g/dL). Fluid ADA was positive. Cross sectional imaging of the abdomen showed omental caking, peritoneal lining nodularity, and hepatosplenomegaly. Fine needle aspiration of the peritoneum showed necrotizing and non-necrotizing granulomas. Sputum gram stain was negative for acid fast bacilli although sputum and ascites cultures ultimately grew TB.
The patient was started on rifampin, isoniazid, pyrazinamide and ethambutol for TB and abstained from further alcohol use. Three months after discharge, jaundice and ascites had resolved and his liver tests had significantly improved.
Discussion: TB peritonitis makes up 4-10% of extrapulmonary TB infections. Though rare in the US, it has a high mortality rate (50-60%). Diagnosis can be complicated by difficulty isolating the organism and culture results can take weeks. TB peritonitis can be supported by ascites fluid studies with elevated lymphocyte count, total protein, and positive ADA; although for more definitive diagnosis peritoneal biopsy should be considered.
This patient represents a unique confluence of portal hypertension related ascites, induced by acute alcoholic hepatitis, along with TB peritonitis. It is possible that transient immunosuppression from alcoholic hepatitis served as a risk factor in reactivation and dissemination of latent TB. An index of suspicion for TB infection, based on his foreign birth, along with his abnormal ascites fluid studies, led to the peritoneal biopsy and ultimate culture diagnosis of his infection that might otherwise have been overlooked.
Disclosures:
Katya Swarts, MD1, Leland Stratton, MD2, Anuragh R. Gudur, MD1, Stephen Caldwell, MD2. B0564 - Acute Alcoholic Hepatitis With Portal Hypertension Complicated by Tuberculous Peritonitis and Ascites, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Katya Swarts, MD1, Leland Stratton, MD2, Anuragh R. Gudur, MD1, Stephen Caldwell, MD2
1University of Virginia Health System, Charlottesville, VA; 2University of Virginia, Charlottesville, VA
Introduction: Peritonitis related to tuberculosis (TB) infection is rare in the US and normally associated with immunocompromised states. We present a patient found to have TB peritonitis during evaluation of alcoholic hepatitis without evident lung disease.
Case Description/Methods: The patient is a 39 yo male born in Mexico with no medical history who presented with three days of abdominal distention, jaundice, and fevers in the setting of alcohol use disorder. He had no other historic risk factors for TB or cough. Exam was remarkable for a distended abdomen. Laboratory results showed leukocytosis, total bilirubin 3.5 (mg/dL), alkaline phosphatase 295 (U/L), AST 147 (U/L), ALT 62 (U/L), and positive quantiferon gold. Chest x-ray had no pulmonary lesions. Ascites fluid studies were significant for high white count (2214 k/uL) with lymphocytic predominance (91%). The serum ascites albumin gradient was consistent with portal hypertension, and ascites total protein was elevated (3.6 g/dL). Fluid ADA was positive. Cross sectional imaging of the abdomen showed omental caking, peritoneal lining nodularity, and hepatosplenomegaly. Fine needle aspiration of the peritoneum showed necrotizing and non-necrotizing granulomas. Sputum gram stain was negative for acid fast bacilli although sputum and ascites cultures ultimately grew TB.
The patient was started on rifampin, isoniazid, pyrazinamide and ethambutol for TB and abstained from further alcohol use. Three months after discharge, jaundice and ascites had resolved and his liver tests had significantly improved.
Discussion: TB peritonitis makes up 4-10% of extrapulmonary TB infections. Though rare in the US, it has a high mortality rate (50-60%). Diagnosis can be complicated by difficulty isolating the organism and culture results can take weeks. TB peritonitis can be supported by ascites fluid studies with elevated lymphocyte count, total protein, and positive ADA; although for more definitive diagnosis peritoneal biopsy should be considered.
This patient represents a unique confluence of portal hypertension related ascites, induced by acute alcoholic hepatitis, along with TB peritonitis. It is possible that transient immunosuppression from alcoholic hepatitis served as a risk factor in reactivation and dissemination of latent TB. An index of suspicion for TB infection, based on his foreign birth, along with his abnormal ascites fluid studies, led to the peritoneal biopsy and ultimate culture diagnosis of his infection that might otherwise have been overlooked.
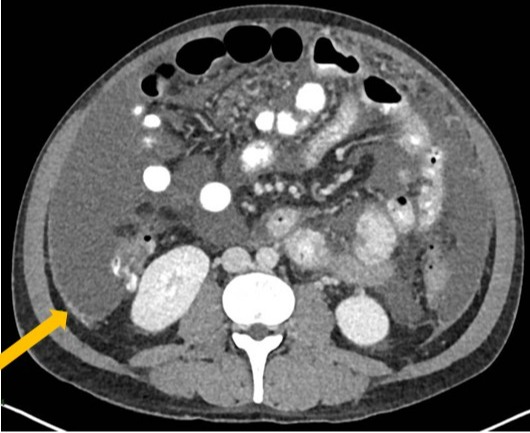
Figure: Nodularity of the peritoneal lining.
Disclosures:
Katya Swarts indicated no relevant financial relationships.
Leland Stratton indicated no relevant financial relationships.
Anuragh Gudur indicated no relevant financial relationships.
Stephen Caldwell: Akero – Grant/Research Support. Avanos – Royalties. BMS – Grant/Research Support. Durect – Grant/Research Support. Exact – Grant/Research Support. Galectin – Grant/Research Support. Galmed – Grant/Research Support. GenFit – Grant/Research Support. Gilead – Grant/Research Support. Inventiva – Grant/Research Support. Madrigal – Grant/Research Support. Target – Grant/Research Support. Zydus – Grant/Research Support.
Katya Swarts, MD1, Leland Stratton, MD2, Anuragh R. Gudur, MD1, Stephen Caldwell, MD2. B0564 - Acute Alcoholic Hepatitis With Portal Hypertension Complicated by Tuberculous Peritonitis and Ascites, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

