Back

Poster Session B - Monday Morning
Category: GI Bleeding
B0345 - Ischemic Gastropathy in a Patient With Severe COVID-19
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Jennifer Hou, MD, PhD
Scripps Clinic
La Jolla, CA
Presenting Author(s)
Jennifer Hou, MD, PhD1, Pooja Magavi, MD2, Shazia M. Jamil, MD1, Fouad J. Moawad, MD, FACG1, Quan M. Nhu, MD, PhD3
1Scripps Clinic, San Diego, CA; 2Scripps Clinic, La Jolla, CA; 3Scripps Clinic & Scripps Research, San Diego, CA
Introduction: The stomach is supplied by an extensive vascular network derived from the celiac axis and its branches, which include the splenic, common hepatic and left gastric arteries. As a result, gastric ischemia occurs infrequently. It can manifest as gastrointestinal (GI) bleeding and has been associated with significant mortality. We present herein a case of ischemic gastropathy in the setting of severe COVID-19.
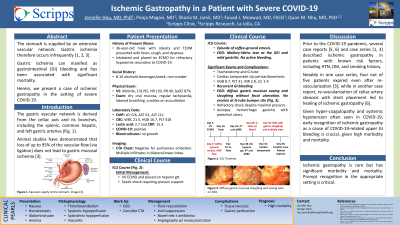
Case Description/Methods: A 36-year-old obese male with newly diagnosed diabetes mellitus type 2 was hospitalized for severe COVID-19 pneumonia. He was initiated on veno-venous extracorporeal membrane oxygenation and anticoagulated on heparin, complicated by coffee-ground emesis. Esophagogastroduodenoscopy (EGD) showed a small Mallory-Weiss tear at the gastroesophageal junction and mild gastritis. Hospital course was complicated by sepsis, shock, acute respiratory distress syndrome and persistent respiratory failure requiring tracheostomy and percutaneous gastrostomy (G-tube), cardiac tamponade requiring pericardiocentesis, renal failure managed with continuous renal replacement therapy, and non-heparin-induced thrombocytopenia refractory to platelet transfusions. One month after G-tube placement, patient developed recurrent GI bleeding with melena, with lab studies showing hemoglobin 8.7 g/dL, platelet 31 K/µL, INR 2.8, BUN 31 mg/dL, and Cr 1.4 mg/dL. EGD demonstrated diffuse gastric mucosal oozing and sloughing without focal ulceration (Figure 1). Due to refractory shock despite maximal pressors, patient was ultimately transitioned to comfort care and expired. Autopsy revealed hemorrhagic gastritis with petechial ulcers.
Discussion: Gastric ischemia and upper GI mucosal injuries including ulcers, erosive gastro-duodenopathy and hemorrhagic gastropathy are some GI complications of COVID-19 that may be mediated by direct viral cytopathic effects and vascular insufficiency. The stomach has a redundant arterial blood supply that is usually protective against ischemic injury. However, states of systemic hypoperfusion, shock, splanchnic hypoperfusion, or thrombosis can precipitate ischemic gastropathy. EGD can be diagnostic and helps assess the extent of ischemia. Medical management should address the underlying cause and is supportive, involving bowel rest, acid suppression and antibiotic therapy. Angiography with revascularization may be considered in cases of vessel occlusion. Potential complications of gastric ischemia include tissue necrosis and gastric perforation. Overall prognosis is poor.
Disclosures:
Jennifer Hou, MD, PhD1, Pooja Magavi, MD2, Shazia M. Jamil, MD1, Fouad J. Moawad, MD, FACG1, Quan M. Nhu, MD, PhD3. B0345 - Ischemic Gastropathy in a Patient With Severe COVID-19, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Scripps Clinic, San Diego, CA; 2Scripps Clinic, La Jolla, CA; 3Scripps Clinic & Scripps Research, San Diego, CA
Introduction: The stomach is supplied by an extensive vascular network derived from the celiac axis and its branches, which include the splenic, common hepatic and left gastric arteries. As a result, gastric ischemia occurs infrequently. It can manifest as gastrointestinal (GI) bleeding and has been associated with significant mortality. We present herein a case of ischemic gastropathy in the setting of severe COVID-19.
Case Description/Methods: A 36-year-old obese male with newly diagnosed diabetes mellitus type 2 was hospitalized for severe COVID-19 pneumonia. He was initiated on veno-venous extracorporeal membrane oxygenation and anticoagulated on heparin, complicated by coffee-ground emesis. Esophagogastroduodenoscopy (EGD) showed a small Mallory-Weiss tear at the gastroesophageal junction and mild gastritis. Hospital course was complicated by sepsis, shock, acute respiratory distress syndrome and persistent respiratory failure requiring tracheostomy and percutaneous gastrostomy (G-tube), cardiac tamponade requiring pericardiocentesis, renal failure managed with continuous renal replacement therapy, and non-heparin-induced thrombocytopenia refractory to platelet transfusions. One month after G-tube placement, patient developed recurrent GI bleeding with melena, with lab studies showing hemoglobin 8.7 g/dL, platelet 31 K/µL, INR 2.8, BUN 31 mg/dL, and Cr 1.4 mg/dL. EGD demonstrated diffuse gastric mucosal oozing and sloughing without focal ulceration (Figure 1). Due to refractory shock despite maximal pressors, patient was ultimately transitioned to comfort care and expired. Autopsy revealed hemorrhagic gastritis with petechial ulcers.
Discussion: Gastric ischemia and upper GI mucosal injuries including ulcers, erosive gastro-duodenopathy and hemorrhagic gastropathy are some GI complications of COVID-19 that may be mediated by direct viral cytopathic effects and vascular insufficiency. The stomach has a redundant arterial blood supply that is usually protective against ischemic injury. However, states of systemic hypoperfusion, shock, splanchnic hypoperfusion, or thrombosis can precipitate ischemic gastropathy. EGD can be diagnostic and helps assess the extent of ischemia. Medical management should address the underlying cause and is supportive, involving bowel rest, acid suppression and antibiotic therapy. Angiography with revascularization may be considered in cases of vessel occlusion. Potential complications of gastric ischemia include tissue necrosis and gastric perforation. Overall prognosis is poor.
Figure: Figure 1. Diffuse gastric mucosal sloughing and oozing seen on EGD.
Disclosures:
Jennifer Hou indicated no relevant financial relationships.
Pooja Magavi indicated no relevant financial relationships.
Shazia Jamil indicated no relevant financial relationships.
Fouad Moawad: Regeneron/Sanofi – Advisory Committee/Board Member, Consultant. Takeda – Advisory Committee/Board Member, Consultant, Speakers Bureau.
Quan Nhu: Cancer Expert Now – Consultant. Regeneron – Speakers Bureau. Sanofi – Advisory Committee/Board Member. Takeda – Advisory Committee/Board Member.
Jennifer Hou, MD, PhD1, Pooja Magavi, MD2, Shazia M. Jamil, MD1, Fouad J. Moawad, MD, FACG1, Quan M. Nhu, MD, PhD3. B0345 - Ischemic Gastropathy in a Patient With Severe COVID-19, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

