Back


Poster Session C - Monday Afternoon
Category: Liver
C0491 - The Impact of Social Determinants of Health on Survival and Disease Severity in Patients With Hepatocellular Carcinoma
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Has Audio
- BF
Bassem Farah, MD
Henry Ford Health System
Detroit, MI
Presenting Author(s)
Bassem Farah, MD, Ahila Manivannan, MD, Kevin Harris, MD, Reena Salgia, MD, Jesse Michelle, PhD, Pin Li, PhD
Henry Ford Health System, Detroit, MI
Introduction: While progress has been made in understanding the medical risk factors for hepatocellular carcinoma (HCC), there is still a dearth of data on social risk factors. While racial and income disparities have been studied, less is known about other social determinants of health (SDOH). We aimed to determine the associations between SDOH of patients diagnosed with HCC leading to lower overall survival and more advanced disease at presentation.
Methods: We conducted a retrospective study from a REDCAP database of patients diagnosed with HCC at our tertiary care center from 2015 to 2019. Body mass index (BMI), gender, marital status, race, insurance status, surveillance status for HCC, education level, transportation method, and veteran status were included as SDOH. Outcomes measured included survival, BCLC (Barcelona Clinic Liver Cancer) stage, tumor size, and presence of metastasis at diagnosis. Using multiple imputation for missing data, multivariate analyses examined these SDOH variables on HCC outcomes.
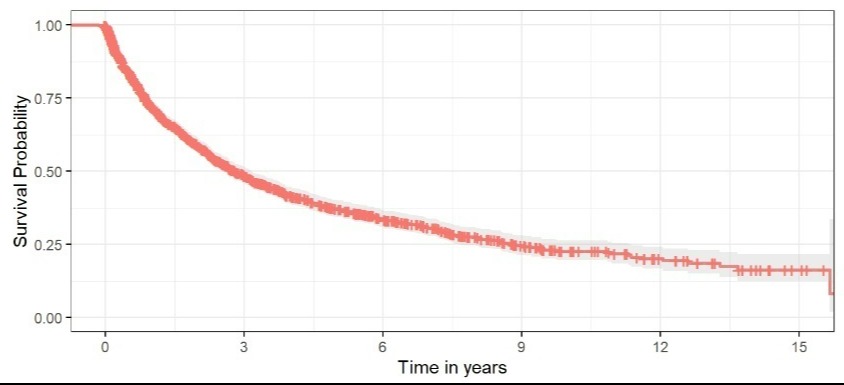
Results: In our cohort of 1655 patients, 73.5% were male and 64.8% were Caucasian. Our cohort is unique given the large number of patients (43.7%) with Medicare or Medicaid as primary insurers. Overall survival was 48.5% at 3 years and 37.3% at 5 years matching national outcomes (Figure 1). Patients who received surveillance prior to HCC diagnosis (HR 0.73, p < 0.005), were married (HR 0.82, p=0.005) and qualified for first-line HCC treatment (HR 0.46, p< 0.005) were associated with better overall survival. Female patients (HR 0.71, p 0.003) were found to have lower BCLC staging at time of diagnosis, but none of the other predictors were significant. Patients who were female (HR 0.76, p=0.032), married (HR 0.79, p=0.044), and had routine surveillance for HCC prior to diagnosis (HR 0.75, p=0.019) were less likely to have an HCC lesion >5 cm. Interestingly, at the time of diagnosis patients with private insurance were more likely to have metastatic HCC (HR 3.43, p< 0.005). Patients with no insurance (HR 0.34, p=0.037), surveillance for HCC prior to diagnosis (HR 0.09, p< 0.005), and at least some college education (HR 0.97, p=0.045) were less likely to have metastatic HCC.
Discussion: Certain SDOH at diagnosis, namely gender, marital status, and surveillance were associated with improved overall survival and earlier HCC diagnosis. However, there were also unexpected findings of those who presented with metastatic disease, necessitating further investigation to understand the underlying factors.
Disclosures:
Bassem Farah, MD, Ahila Manivannan, MD, Kevin Harris, MD, Reena Salgia, MD, Jesse Michelle, PhD, Pin Li, PhD. C0491 - The Impact of Social Determinants of Health on Survival and Disease Severity in Patients With Hepatocellular Carcinoma, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Henry Ford Health System, Detroit, MI
Introduction: While progress has been made in understanding the medical risk factors for hepatocellular carcinoma (HCC), there is still a dearth of data on social risk factors. While racial and income disparities have been studied, less is known about other social determinants of health (SDOH). We aimed to determine the associations between SDOH of patients diagnosed with HCC leading to lower overall survival and more advanced disease at presentation.
Methods: We conducted a retrospective study from a REDCAP database of patients diagnosed with HCC at our tertiary care center from 2015 to 2019. Body mass index (BMI), gender, marital status, race, insurance status, surveillance status for HCC, education level, transportation method, and veteran status were included as SDOH. Outcomes measured included survival, BCLC (Barcelona Clinic Liver Cancer) stage, tumor size, and presence of metastasis at diagnosis. Using multiple imputation for missing data, multivariate analyses examined these SDOH variables on HCC outcomes.
Results: In our cohort of 1655 patients, 73.5% were male and 64.8% were Caucasian. Our cohort is unique given the large number of patients (43.7%) with Medicare or Medicaid as primary insurers. Overall survival was 48.5% at 3 years and 37.3% at 5 years matching national outcomes (Figure 1). Patients who received surveillance prior to HCC diagnosis (HR 0.73, p < 0.005), were married (HR 0.82, p=0.005) and qualified for first-line HCC treatment (HR 0.46, p< 0.005) were associated with better overall survival. Female patients (HR 0.71, p 0.003) were found to have lower BCLC staging at time of diagnosis, but none of the other predictors were significant. Patients who were female (HR 0.76, p=0.032), married (HR 0.79, p=0.044), and had routine surveillance for HCC prior to diagnosis (HR 0.75, p=0.019) were less likely to have an HCC lesion >5 cm. Interestingly, at the time of diagnosis patients with private insurance were more likely to have metastatic HCC (HR 3.43, p< 0.005). Patients with no insurance (HR 0.34, p=0.037), surveillance for HCC prior to diagnosis (HR 0.09, p< 0.005), and at least some college education (HR 0.97, p=0.045) were less likely to have metastatic HCC.
Discussion: Certain SDOH at diagnosis, namely gender, marital status, and surveillance were associated with improved overall survival and earlier HCC diagnosis. However, there were also unexpected findings of those who presented with metastatic disease, necessitating further investigation to understand the underlying factors.
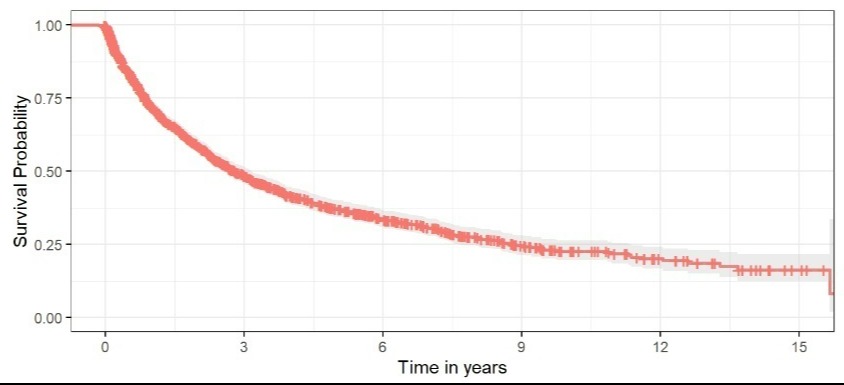
Figure: Figure 1: Kaplan Meier Curve of Overall Survival
Disclosures:
Bassem Farah indicated no relevant financial relationships.
Ahila Manivannan indicated no relevant financial relationships.
Kevin Harris indicated no relevant financial relationships.
Reena Salgia indicated no relevant financial relationships.
Jesse Michelle indicated no relevant financial relationships.
Pin Li indicated no relevant financial relationships.
Bassem Farah, MD, Ahila Manivannan, MD, Kevin Harris, MD, Reena Salgia, MD, Jesse Michelle, PhD, Pin Li, PhD. C0491 - The Impact of Social Determinants of Health on Survival and Disease Severity in Patients With Hepatocellular Carcinoma, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
