Back

Poster Session C - Monday Afternoon
Category: Liver
C0494 - Burden and Independent Predictors of Readmissions in Portal Venous Thrombosis Hospitalizations
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio
Robert Kwei-Nsoro, MD
John H. Stroger, Jr. Hospital of Cook County
Chicago, IL
Presenting Author(s)
Robert Kwei-Nsoro, MD1, Hisham Laswi, MD1, Adewale Adedoyin, MBBS2, Pius E. Ojemolon, MD1, Hafeez Shaka, MD1
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2Englewood Hospital, Englewood, NJ
Introduction: Portal vein thrombosis (PVT) is a relatively rare disease.Reliable data on incidence and prevalence is lacking, autopsy studies have reported a population prevalence of 1 percent.
30-day readmission rates are an indicator of health care quality and delivery. Repeated admissions have a significant impact on the overall cost of health care.This study aimed to outline the burden of PVT readmissions and identify the modifiable predictors of readmissions.
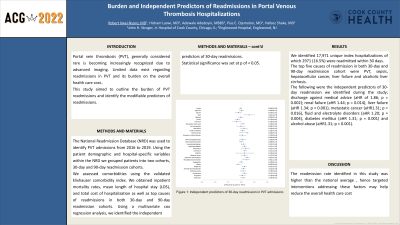
Methods: The National Readmission Database (NRD) was used to identify PVT admissions from 2016 to 2019. Hospitalization of patients less than 18 years and elective admissions were excluded. After identifying our 30-day and 90-day readmission cohorts, we then assessed the patient demographic and hospital-specific variables within the NRD. We also assessed comorbidities using the validated Elixhauser comorbidity index. Outcomes included inpatient mortality rates, mean length of hospital stay (LOS), mean hospitalization cost (THC) and total cost of hospitalization. We also identified the top causes of readmissions in both 30 and 90-day readmission cohorts.Using a multivariate cox regression analysis we identified the independent predictors of 30-day readmissions. Statistical significance was set at p of < 0.05.
Results: A total of 17971 index PVT admissions for 30-day readmission and 14696 index PVT admissions for the 90-day readmissions study were included. Of these, 2971(16.5%) encounters had readmission within 30 days and 3737(25.4%) encounters had readmission within 90 days. The top five causes readmission in both 30-day and 90-day readmission cohort were PVT, sepsis, hepatocellular cancer, liver failure and alcoholic liver cirrhosis. The following were the independent predictors of 30-day readmission we identified during the study; discharge against medical advice-AMA (aHR of 1.86; p=0.002); renal failure (aHR 1.44 p= 0.014),liver failure (aHR 1.34;p < 0.001), metastatic cancer (aHR1.31; p= 0.016), rheumatoid arthritis and collagen vascular disease (aHR 1.48, =p 0.006) fluid and electrolyte disorders (aHR 1.20, p= 0.004), diabetes mellitus (aHR 1.31,p 0.001) and alcohol abuse (aHR1.31;p=< 0.001).
Discussion: The independent predictors of 30-day readmissions identified during this study, are of clinical relevance because of their association with potentially reversible readmissions.Some of these conditions can be optimized before discharge and some respond to effective out-patient management.
Disclosures:
Robert Kwei-Nsoro, MD1, Hisham Laswi, MD1, Adewale Adedoyin, MBBS2, Pius E. Ojemolon, MD1, Hafeez Shaka, MD1. C0494 - Burden and Independent Predictors of Readmissions in Portal Venous Thrombosis Hospitalizations, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2Englewood Hospital, Englewood, NJ
Introduction: Portal vein thrombosis (PVT) is a relatively rare disease.Reliable data on incidence and prevalence is lacking, autopsy studies have reported a population prevalence of 1 percent.
30-day readmission rates are an indicator of health care quality and delivery. Repeated admissions have a significant impact on the overall cost of health care.This study aimed to outline the burden of PVT readmissions and identify the modifiable predictors of readmissions.
Methods: The National Readmission Database (NRD) was used to identify PVT admissions from 2016 to 2019. Hospitalization of patients less than 18 years and elective admissions were excluded. After identifying our 30-day and 90-day readmission cohorts, we then assessed the patient demographic and hospital-specific variables within the NRD. We also assessed comorbidities using the validated Elixhauser comorbidity index. Outcomes included inpatient mortality rates, mean length of hospital stay (LOS), mean hospitalization cost (THC) and total cost of hospitalization. We also identified the top causes of readmissions in both 30 and 90-day readmission cohorts.Using a multivariate cox regression analysis we identified the independent predictors of 30-day readmissions. Statistical significance was set at p of < 0.05.
Results: A total of 17971 index PVT admissions for 30-day readmission and 14696 index PVT admissions for the 90-day readmissions study were included. Of these, 2971(16.5%) encounters had readmission within 30 days and 3737(25.4%) encounters had readmission within 90 days. The top five causes readmission in both 30-day and 90-day readmission cohort were PVT, sepsis, hepatocellular cancer, liver failure and alcoholic liver cirrhosis. The following were the independent predictors of 30-day readmission we identified during the study; discharge against medical advice-AMA (aHR of 1.86; p=0.002); renal failure (aHR 1.44 p= 0.014),liver failure (aHR 1.34;p < 0.001), metastatic cancer (aHR1.31; p= 0.016), rheumatoid arthritis and collagen vascular disease (aHR 1.48, =p 0.006) fluid and electrolyte disorders (aHR 1.20, p= 0.004), diabetes mellitus (aHR 1.31,p 0.001) and alcohol abuse (aHR1.31;p=< 0.001).
Discussion: The independent predictors of 30-day readmissions identified during this study, are of clinical relevance because of their association with potentially reversible readmissions.Some of these conditions can be optimized before discharge and some respond to effective out-patient management.
Disclosures:
Robert Kwei-Nsoro indicated no relevant financial relationships.
Hisham Laswi indicated no relevant financial relationships.
Adewale Adedoyin indicated no relevant financial relationships.
Pius Ojemolon indicated no relevant financial relationships.
Hafeez Shaka indicated no relevant financial relationships.
Robert Kwei-Nsoro, MD1, Hisham Laswi, MD1, Adewale Adedoyin, MBBS2, Pius E. Ojemolon, MD1, Hafeez Shaka, MD1. C0494 - Burden and Independent Predictors of Readmissions in Portal Venous Thrombosis Hospitalizations, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
