Back

Poster Session B - Monday Morning
Category: GI Bleeding
B0332 - Intestinal Endometriosis Leading to Recurrent Hematochezia
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Marta Arjonilla, MD
Stony Brook Medicine
Stony Brook, NY
Presenting Author(s)
Award: Presidential Poster Award
Marta Arjonilla, MD1, Amrin Khander, MD2, Timothy Pal, MD1, Daniel S. Jamorabo, MD1
1Stony Brook Medicine, Stony Brook, NY; 2Weill Cornell Medical College, New York, NY
Introduction: Endometriosis involves the GI tract in about 5.4% of all endometriosis cases. This leads to non-specific symptoms such as changes in stool consistency, abdominal pain, and hematochezia, though most women remain asymptomatic. The diagnosis of intestinal endometriosis requires high clinical suspicion. There is no step-wise approach to the workup and the gold standard for diagnosis remains histopathological.
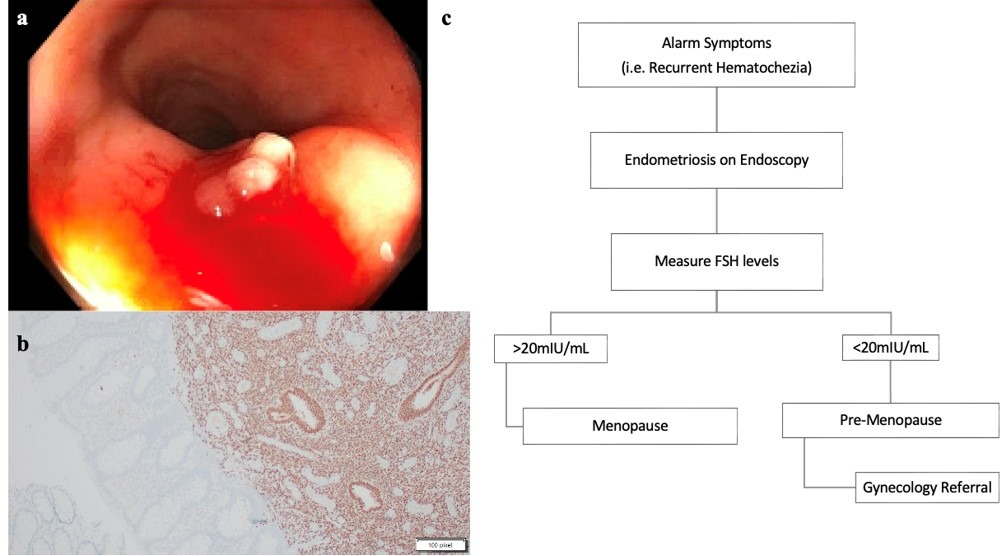
Case Description/Methods: 51F presented for intermittent rectal pain and hematochezia for the preceding two months. She underwent a vaginal hysterectomy without oophorectomy 11 years prior for an unclear indication. Her gynecologist did a transvaginal ultrasound (TVUS) that revealed no acute abnormality. Clinical examination showed tenderness with passage of finger without blood or anal fissures. The colonoscopy revealed a 7mm sessile polyp in the sigmoid colon (Figure 1a). The histopathology showed no cytologic or architectural atypia, but an immunohistochemical stain for CD10 highlighted the stromal cells as endometrial-type, which supported intestinal endometriosis (Figure 1b). Given she still had her ovaries, a follicle stimulating hormone (FSH) level was sent to confirm her menopause status. Her FSH was elevated to 56.6mIU/mL (post-menopausal FSH is >20mIU/mL). The patient exhibited no further rectal pain and hematochezia after removal of the endometrial tissue from the colon. Given the absence of other possible etiologies and resolution of symptoms, we attributed her hematochezia to endometriosis.
Discussion: Endometriosis is defined as the presence of functioning endometrial glands and stroma outside the uterine cavity. In a patient without known endometriosis or a prior hysterectomy, intermittent rectal bleeding would prompt a GI work-up rather than a gynecological work-up. A colonoscopy with biopsy would be warranted and required to identify and confirm endometrial tissue in the GI tract.
This case is particularly unique as the patient was asymptomatic from her endometriosis during her reproductive years and presented in the post-menopausal state. Menopause is a low-estrogen state, however the decreased levels in menopause are enough to cause symptoms. Furthermore, our patient was overweight and since estrogen can be synthesized in adipose tissue, her risk of symptoms from endometriosis was further increased. As such, we advise our gastroenterology colleagues to keep endometriosis is mind as a possible cause of GI tract bleeding, even in the post-menopausal population (Figure 1c).
Disclosures:
Marta Arjonilla, MD1, Amrin Khander, MD2, Timothy Pal, MD1, Daniel S. Jamorabo, MD1. B0332 - Intestinal Endometriosis Leading to Recurrent Hematochezia, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Marta Arjonilla, MD1, Amrin Khander, MD2, Timothy Pal, MD1, Daniel S. Jamorabo, MD1
1Stony Brook Medicine, Stony Brook, NY; 2Weill Cornell Medical College, New York, NY
Introduction: Endometriosis involves the GI tract in about 5.4% of all endometriosis cases. This leads to non-specific symptoms such as changes in stool consistency, abdominal pain, and hematochezia, though most women remain asymptomatic. The diagnosis of intestinal endometriosis requires high clinical suspicion. There is no step-wise approach to the workup and the gold standard for diagnosis remains histopathological.
Case Description/Methods: 51F presented for intermittent rectal pain and hematochezia for the preceding two months. She underwent a vaginal hysterectomy without oophorectomy 11 years prior for an unclear indication. Her gynecologist did a transvaginal ultrasound (TVUS) that revealed no acute abnormality. Clinical examination showed tenderness with passage of finger without blood or anal fissures. The colonoscopy revealed a 7mm sessile polyp in the sigmoid colon (Figure 1a). The histopathology showed no cytologic or architectural atypia, but an immunohistochemical stain for CD10 highlighted the stromal cells as endometrial-type, which supported intestinal endometriosis (Figure 1b). Given she still had her ovaries, a follicle stimulating hormone (FSH) level was sent to confirm her menopause status. Her FSH was elevated to 56.6mIU/mL (post-menopausal FSH is >20mIU/mL). The patient exhibited no further rectal pain and hematochezia after removal of the endometrial tissue from the colon. Given the absence of other possible etiologies and resolution of symptoms, we attributed her hematochezia to endometriosis.
Discussion: Endometriosis is defined as the presence of functioning endometrial glands and stroma outside the uterine cavity. In a patient without known endometriosis or a prior hysterectomy, intermittent rectal bleeding would prompt a GI work-up rather than a gynecological work-up. A colonoscopy with biopsy would be warranted and required to identify and confirm endometrial tissue in the GI tract.
This case is particularly unique as the patient was asymptomatic from her endometriosis during her reproductive years and presented in the post-menopausal state. Menopause is a low-estrogen state, however the decreased levels in menopause are enough to cause symptoms. Furthermore, our patient was overweight and since estrogen can be synthesized in adipose tissue, her risk of symptoms from endometriosis was further increased. As such, we advise our gastroenterology colleagues to keep endometriosis is mind as a possible cause of GI tract bleeding, even in the post-menopausal population (Figure 1c).
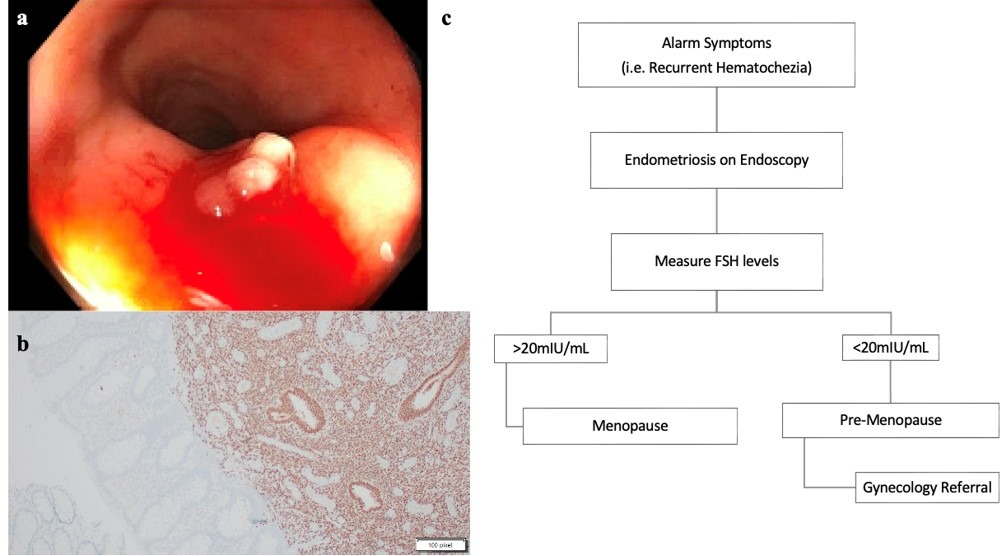
Figure: Figure 1a: Colonoscopic view of a hyper-vascular lesion embedded at the sigmoid colon wall lumen; 1b: Immunohistochemical stain (brown chromogen) for CD10 expression highlights the cytoplasm of stromal cells as endometrial type stroma. The stain for CD10 delineate a clear demarcation between the endometriosis and the colonic lamina propria; 1c: Proposed algorithm for Gastroenterologist when endometriosis is diagnosed via colonoscopy.
Disclosures:
Marta Arjonilla indicated no relevant financial relationships.
Amrin Khander indicated no relevant financial relationships.
Timothy Pal indicated no relevant financial relationships.
Daniel Jamorabo indicated no relevant financial relationships.
Marta Arjonilla, MD1, Amrin Khander, MD2, Timothy Pal, MD1, Daniel S. Jamorabo, MD1. B0332 - Intestinal Endometriosis Leading to Recurrent Hematochezia, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.


