Back

Poster Session B - Monday Morning
Category: Esophagus
B0230 - Use of Upadacitinib in Refractory Esophageal Lichen Planus: Endoscopic Improvement in "Planus" Sight
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- EB
Erica C. Becker, MD, MPH
University of Connecticut Health Center
Farmington, CT
Presenting Author(s)
Award: Presidential Poster Award
Erica C. Becker, MD, MPH1, Marianna G. Mavilia, DO1, Justin Finch, MD2, Mingfu Yu, MD, MS1, Houman Rezaizadeh, MD1
1University of Connecticut Health Center, Farmington, CT; 2Central CT Dermatology, Cromwell, CT
Introduction: Lichen planus (LP) is an inflammatory skin condition that affects oropharyngeal and esophageal mucosa. Esophageal LP (ELP) has a prevalence of 0.19% but is thought to be underdiagnosed. It presents with ulceration, exudates, rings and/or strictures. Although pathogenesis of LP is incompletely understood, the JAK signaling pathway is thought to play a role. Upadacitinib is a selective JAK1 inhibitor approved for use in ulcerative colitis. We present a case of refractory ELP with endoscopic and histologic response to upadacitinib after failing standard treatment.
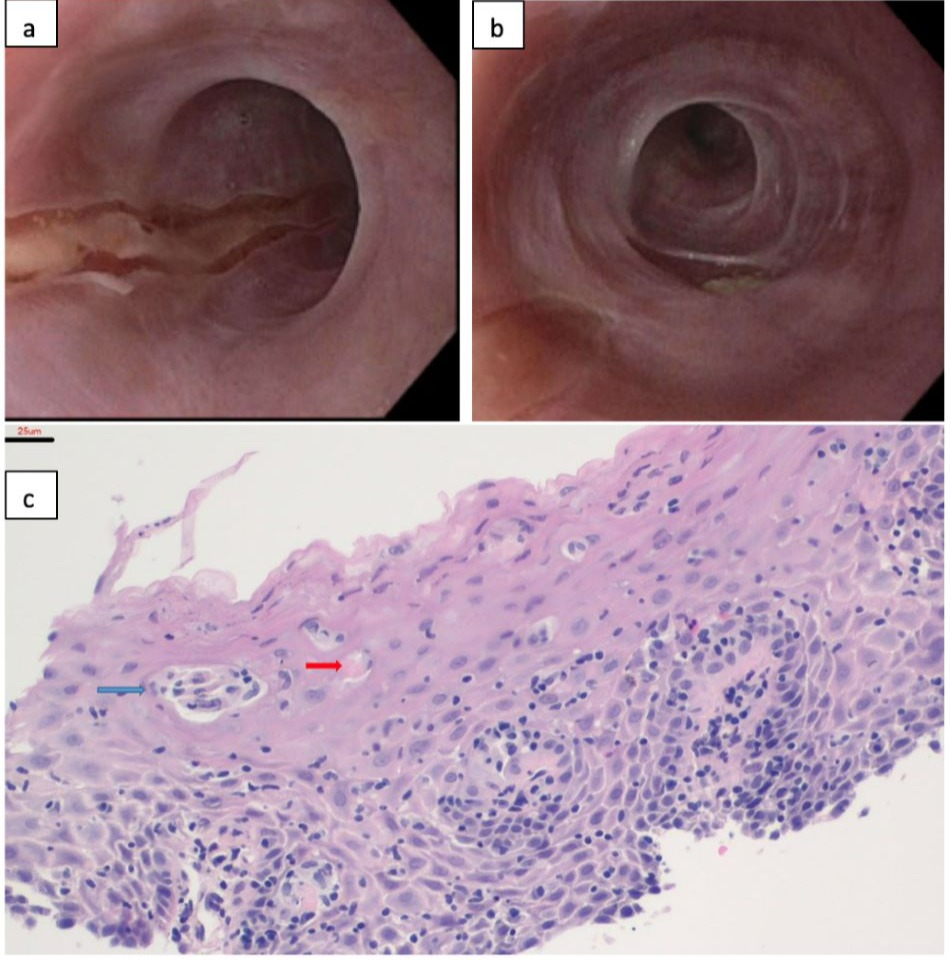
Case Description/Methods: A 68 year old female with history of Sjogren’s syndrome, LP, and prior peptic stricture at the gastroesophageal junction presented with dysphagia to both liquids and solids, intermittent reflux, regurgitation, and self-limited impactions. An EGD showed esophageal stenosis, severe esophagitis, and mucosal ulceration (Fig. 1a). Passage of the scope resulted in dilation; however, formal dilation of stenosis was not performed due to severity of esophagitis. Esophageal biopsies revealed squamous mucosa with parakeratosis, dyskeratotic cells and scattered lymphocytes consistent with ELP. Subsequently, the patient recalled having a remote history of oral lichen planus. She was started on pantoprazole 40 mg twice daily and budesonide oral slurry with limited response. With co-management by gastroenterology and dermatology, she was initiated on mycophenolate 500 mg daily and increased to 2000 mg twice a day. She continued to lack both histologic and symptomatic improvement remaining limited to a soft and liquid diet resulting in a 20lb weight loss. She was started on monotherapy with upadacitinib 30 mg twice daily. This resulted in marked symptomatic recovery with repeat endoscopy 3 months later showing dramatic macroscopic and histologic improvement (Fig. 1b), with only some residual fibrostenotic disease remaining (Fig. 1c).
Discussion: Multimodal treatment is typically employed in ELP with medical therapy and endoscopic dilation. Systemic or topical steroids are first line, with efficacy estimated at 60-70%. Other therapies include tacrolimus, cyclosporine, mycophenolate, rituximab, adalimumab, and tofacitinib, however data for these therapies are limited. To date, there are only two cases reported in the literature of successful treatment of oro-esophageal LP with upadacitinib. Given profound improvement seen in our patient, upadacitinib may offer another alternative for these difficult-to-treat patients.
Disclosures:
Erica C. Becker, MD, MPH1, Marianna G. Mavilia, DO1, Justin Finch, MD2, Mingfu Yu, MD, MS1, Houman Rezaizadeh, MD1. B0230 - Use of Upadacitinib in Refractory Esophageal Lichen Planus: Endoscopic Improvement in "Planus" Sight, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Erica C. Becker, MD, MPH1, Marianna G. Mavilia, DO1, Justin Finch, MD2, Mingfu Yu, MD, MS1, Houman Rezaizadeh, MD1
1University of Connecticut Health Center, Farmington, CT; 2Central CT Dermatology, Cromwell, CT
Introduction: Lichen planus (LP) is an inflammatory skin condition that affects oropharyngeal and esophageal mucosa. Esophageal LP (ELP) has a prevalence of 0.19% but is thought to be underdiagnosed. It presents with ulceration, exudates, rings and/or strictures. Although pathogenesis of LP is incompletely understood, the JAK signaling pathway is thought to play a role. Upadacitinib is a selective JAK1 inhibitor approved for use in ulcerative colitis. We present a case of refractory ELP with endoscopic and histologic response to upadacitinib after failing standard treatment.
Case Description/Methods: A 68 year old female with history of Sjogren’s syndrome, LP, and prior peptic stricture at the gastroesophageal junction presented with dysphagia to both liquids and solids, intermittent reflux, regurgitation, and self-limited impactions. An EGD showed esophageal stenosis, severe esophagitis, and mucosal ulceration (Fig. 1a). Passage of the scope resulted in dilation; however, formal dilation of stenosis was not performed due to severity of esophagitis. Esophageal biopsies revealed squamous mucosa with parakeratosis, dyskeratotic cells and scattered lymphocytes consistent with ELP. Subsequently, the patient recalled having a remote history of oral lichen planus. She was started on pantoprazole 40 mg twice daily and budesonide oral slurry with limited response. With co-management by gastroenterology and dermatology, she was initiated on mycophenolate 500 mg daily and increased to 2000 mg twice a day. She continued to lack both histologic and symptomatic improvement remaining limited to a soft and liquid diet resulting in a 20lb weight loss. She was started on monotherapy with upadacitinib 30 mg twice daily. This resulted in marked symptomatic recovery with repeat endoscopy 3 months later showing dramatic macroscopic and histologic improvement (Fig. 1b), with only some residual fibrostenotic disease remaining (Fig. 1c).
Discussion: Multimodal treatment is typically employed in ELP with medical therapy and endoscopic dilation. Systemic or topical steroids are first line, with efficacy estimated at 60-70%. Other therapies include tacrolimus, cyclosporine, mycophenolate, rituximab, adalimumab, and tofacitinib, however data for these therapies are limited. To date, there are only two cases reported in the literature of successful treatment of oro-esophageal LP with upadacitinib. Given profound improvement seen in our patient, upadacitinib may offer another alternative for these difficult-to-treat patients.
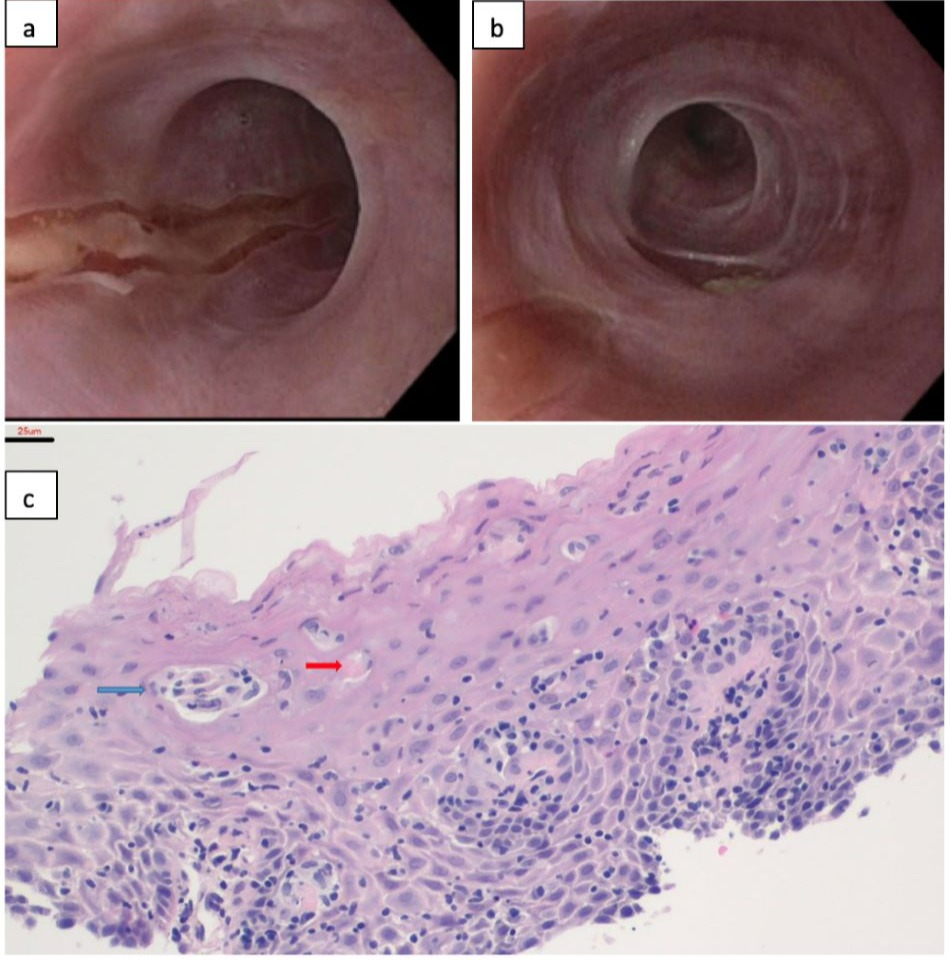
Figure: Figure 1a. ELP on initial diagnostic endoscopy before initiation of therapy. 1b. Follow up endoscopy performed after 12 weeks of upadacitinib treatment. 1c. Lichenoid esophagitis: lymphocytic infiltrates, focal histiocytic aggregate (blue arrow) and dyskeratosis (Civatte body, red arrow).
Disclosures:
Erica Becker indicated no relevant financial relationships.
Marianna Mavilia indicated no relevant financial relationships.
Justin Finch indicated no relevant financial relationships.
Mingfu Yu indicated no relevant financial relationships.
Houman Rezaizadeh: Alexion Pharmaceuticals – Spouse is employee of, Stock Options, Stock-publicly held company(excluding mutual/index funds). AstraZeneca – Spouse is employee of, Stock Options, Stock-publicly held company(excluding mutual/index funds). Celgene/Bristol-Meyers-Squibb – Grant/Research Support. Regeneron – Speakers Bureau. Skope LLC – Advisory Committee/Board Member, Consultant, Stock-privately held company.
Erica C. Becker, MD, MPH1, Marianna G. Mavilia, DO1, Justin Finch, MD2, Mingfu Yu, MD, MS1, Houman Rezaizadeh, MD1. B0230 - Use of Upadacitinib in Refractory Esophageal Lichen Planus: Endoscopic Improvement in "Planus" Sight, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

