Back

Poster Session C - Monday Afternoon
Category: Liver
C0512 - Duodenal Permeability Is Associated With Future Hospitalizations in Patients With Moderately Severe Cirrhosis
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio
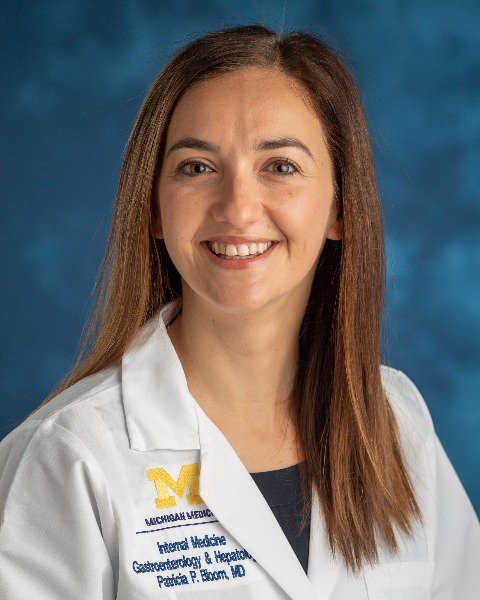
Patricia P. Bloom, MD
Assistant Professor
University of Michigan
Ann Arbor, MI
Presenting Author(s)
Patricia P. Bloom, MD, Krishna Rao, MD, MS, Shi Yi Zhou, PhD, Christine Bassis, PhD, Borko Nojkov, MD, Chung Owyang, MD, Vincent Young, MD, PhD, Anna S. Lok, MD
University of Michigan, Ann Arbor, MI
Introduction: Several complications of cirrhosis result from the translocation of bacteria or their products across the intestinal epithelium. We aimed to assess if intestinal permeability and mucosal bacteria associate with hospitalization in patients with cirrhosis.
Methods: We obtained duodenum, ileum, and colon tissue biopsies from patients with cirrhosis and controls without liver disease. Composition of the mucosal microbiota was determined via 16S rRNA gene sequencing and epithelial permeability assessed by measuring transepithelial electrical resistance (TEER). Outcomes of patients with cirrhosis at 6 months were assessed, with and without stratification by MELD score.
Results: We studied 46 patients with cirrhosis (10 alcohol-related) and 33 controls and obtained 62 duodenum, 31 ileum, and 34 colon biopsies. Patients with cirrhosis were similarly aged to controls (60 vs. 58 years) and had a similar number of extra-hepatic comorbidities (2 vs. 2). Patients with cirrhosis had median MELD 8 (IQR 7, 10); 66% were male. Compared to controls, patients with cirrhosis had lower TEER (i.e., increased epithelial permeability) in the duodenum (12.9 ± 3.4 Ω/cm2 vs. 18.5 ± 7.1 Ω/cm2; P = 0.002) but not in the ileum or colon.
Among the 45 patients with cirrhosis followed for 6 months post-endoscopy, 13 patients were hospitalized, 4 for liver-related diagnoses, and none died.
Duodenal alpha diversity was lower in all patients with cirrhosis who were hospitalized compared to those not hospitalized (inverse Simpson: 5.8 vs. 9.8, P < 0.05).
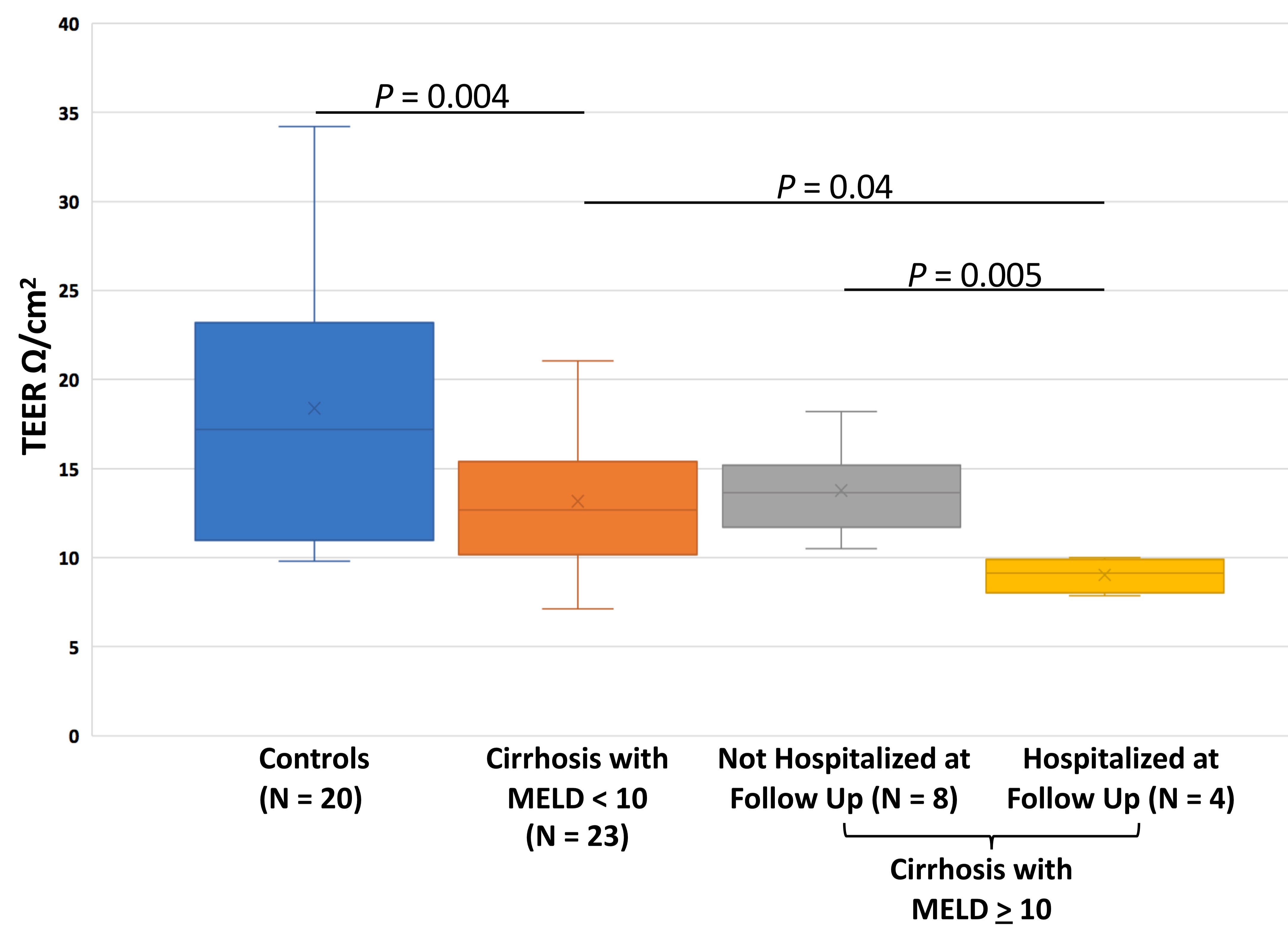
TEER in each gut segment did not predict future hospitalization in the overall cohort of patients with cirrhosis. However, among patients with the highest quartile of MELD (>10; n = 12), duodenal TEER was lower in those who were hospitalized than those not hospitalized (9.0 ± 1.0 Ω/cm2 vs. 13.8 ± 2.5 Ω/cm2, P = 0.005; Figure) and lower in those hospitalized for a liver-related diagnosis than those not hospitalized for a liver-related diagnosis (9.8 ± 0.3 Ω/cm2 vs. 12.7 ± 3.2 Ω/cm2, P = 0.03).
Compared to other etiologies, patients with alcohol-related cirrhosis trended towards lower duodenal TEER (11.3 Ω/cm2 vs. 13.4 Ω/cm2, P = 0.08), even after controlling for MELD.
Discussion: High duodenal epithelial permeability and low mucosa alpha diversity was associated with hospitalization and liver-related hospitalization in patients with moderately severe cirrhosis. Reversal of duodenal permeability may prevent hospitalizations among patients with cirrhosis.
Disclosures:
Patricia P. Bloom, MD, Krishna Rao, MD, MS, Shi Yi Zhou, PhD, Christine Bassis, PhD, Borko Nojkov, MD, Chung Owyang, MD, Vincent Young, MD, PhD, Anna S. Lok, MD. C0512 - Duodenal Permeability Is Associated With Future Hospitalizations in Patients With Moderately Severe Cirrhosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
University of Michigan, Ann Arbor, MI
Introduction: Several complications of cirrhosis result from the translocation of bacteria or their products across the intestinal epithelium. We aimed to assess if intestinal permeability and mucosal bacteria associate with hospitalization in patients with cirrhosis.
Methods: We obtained duodenum, ileum, and colon tissue biopsies from patients with cirrhosis and controls without liver disease. Composition of the mucosal microbiota was determined via 16S rRNA gene sequencing and epithelial permeability assessed by measuring transepithelial electrical resistance (TEER). Outcomes of patients with cirrhosis at 6 months were assessed, with and without stratification by MELD score.
Results: We studied 46 patients with cirrhosis (10 alcohol-related) and 33 controls and obtained 62 duodenum, 31 ileum, and 34 colon biopsies. Patients with cirrhosis were similarly aged to controls (60 vs. 58 years) and had a similar number of extra-hepatic comorbidities (2 vs. 2). Patients with cirrhosis had median MELD 8 (IQR 7, 10); 66% were male. Compared to controls, patients with cirrhosis had lower TEER (i.e., increased epithelial permeability) in the duodenum (12.9 ± 3.4 Ω/cm2 vs. 18.5 ± 7.1 Ω/cm2; P = 0.002) but not in the ileum or colon.
Among the 45 patients with cirrhosis followed for 6 months post-endoscopy, 13 patients were hospitalized, 4 for liver-related diagnoses, and none died.
Duodenal alpha diversity was lower in all patients with cirrhosis who were hospitalized compared to those not hospitalized (inverse Simpson: 5.8 vs. 9.8, P < 0.05).
TEER in each gut segment did not predict future hospitalization in the overall cohort of patients with cirrhosis. However, among patients with the highest quartile of MELD (>10; n = 12), duodenal TEER was lower in those who were hospitalized than those not hospitalized (9.0 ± 1.0 Ω/cm2 vs. 13.8 ± 2.5 Ω/cm2, P = 0.005; Figure) and lower in those hospitalized for a liver-related diagnosis than those not hospitalized for a liver-related diagnosis (9.8 ± 0.3 Ω/cm2 vs. 12.7 ± 3.2 Ω/cm2, P = 0.03).
Compared to other etiologies, patients with alcohol-related cirrhosis trended towards lower duodenal TEER (11.3 Ω/cm2 vs. 13.4 Ω/cm2, P = 0.08), even after controlling for MELD.
Discussion: High duodenal epithelial permeability and low mucosa alpha diversity was associated with hospitalization and liver-related hospitalization in patients with moderately severe cirrhosis. Reversal of duodenal permeability may prevent hospitalizations among patients with cirrhosis.
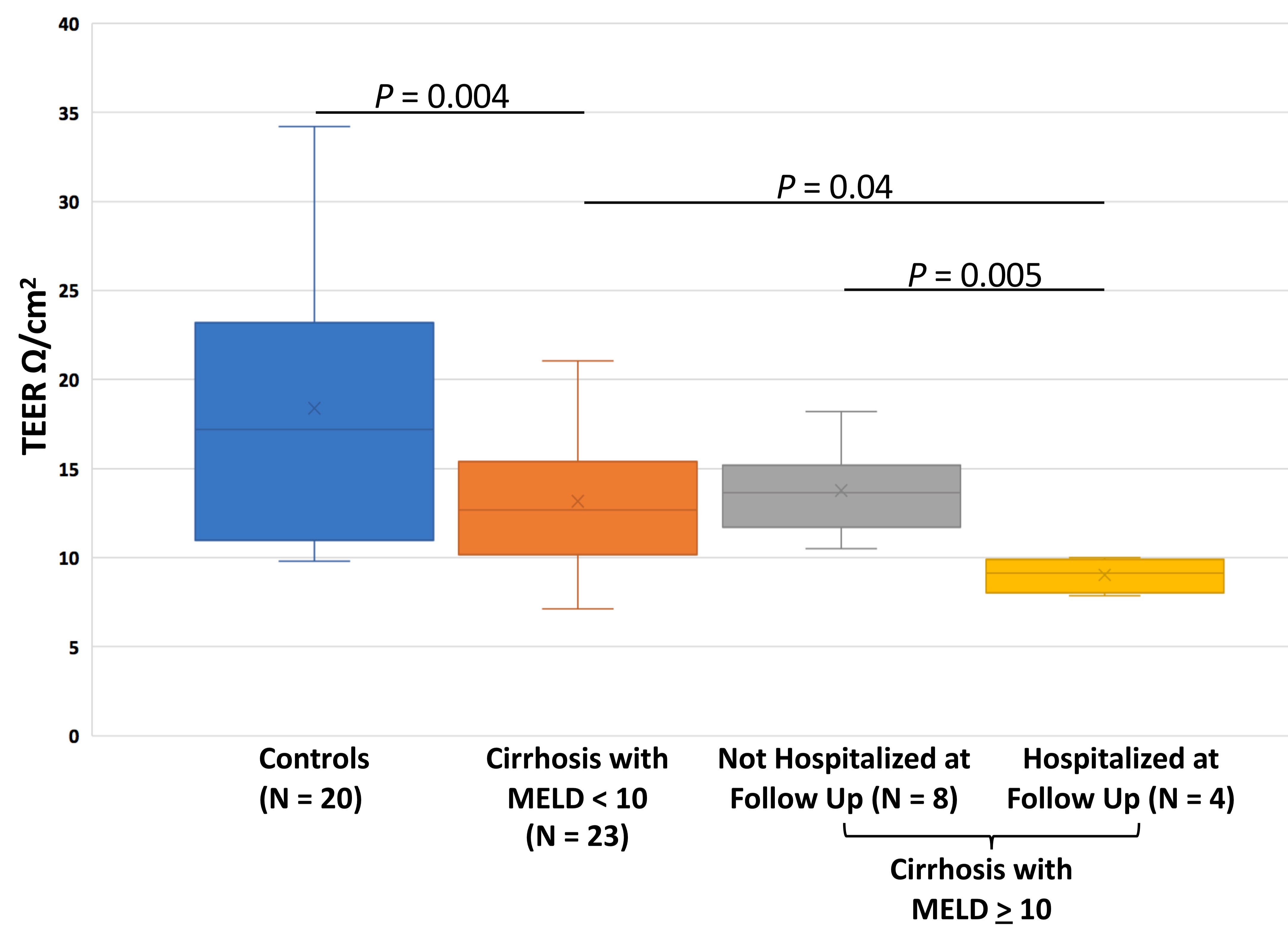
Figure: Duodenal Permeability Varied by Patient Type
Disclosures:
Patricia Bloom: Synlogic Inc – Consultant. Vedanta Biosciences – Grant/Research Support.
Krishna Rao: Merck & Co., Inc. – Grant/Research Support. Seres Therapeutics – Consultant. Summit Therapeutics – Consultant.
Shi Yi Zhou indicated no relevant financial relationships.
Christine Bassis indicated no relevant financial relationships.
Borko Nojkov indicated no relevant financial relationships.
Chung Owyang indicated no relevant financial relationships.
Vincent Young: Vedanta Biosciences – Consultant, Grant/Research Support.
Anna Lok: Novo Nordisk – DSMB chair.
Patricia P. Bloom, MD, Krishna Rao, MD, MS, Shi Yi Zhou, PhD, Christine Bassis, PhD, Borko Nojkov, MD, Chung Owyang, MD, Vincent Young, MD, PhD, Anna S. Lok, MD. C0512 - Duodenal Permeability Is Associated With Future Hospitalizations in Patients With Moderately Severe Cirrhosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
