Back

Poster Session B - Monday Morning
Category: Liver
B0566 - Be Suspicious: A Unique Case of Herpes Simplex Virus Hepatitis
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Yara Dababneh, MD
Henry Ford Hospital
Detroit, MI
Presenting Author(s)
Yara Dababneh, MD1, Aroob Sweidan, MD1, Poornima Oruganti, MD1, Syed-Mohammed Jafri, MD2, Qing Chang, MD1
1Henry Ford Hospital, Detroit, MI; 2Henry Ford Health System, Detroit, MI
Introduction: We present a case of disseminated HSV infection leading to acute liver failure and encephalitis in the setting of a history of autologous stem cell transplant.
Case Description/Methods: A 66-year-old female with a past medical history of amyloidosis status post chemotherapy and autologous stem cell transplant in 2018 and chronic kidney disease was transferred to a tertiary care facility for concern of acute liver failure. On initial presentation, she was encephalopathic. Laboratories demonstrated an AST of 5264 IU/L, ALT of 3237 IU/L, INR of 3.1, and creatinine of 5.92. No other significant personal or family history was found. Workup was negative for toxins.
The patient was considered immunocompromised. Her infectious workup was initially positive for E. coli in urine culture and Fusarium species in respiratory culture. The patient was initially thought to have liver hypoperfusion in the setting of severe sepsis. Serum testing for HSV1 and HSV2 was performed, and the HSV1 qualitative PCR was found to be positive. The patient’s liver enzymes remained elevated. Lumbar puncture was performed, and the patient was initiated on intravenous Acyclovir given a high index of suspicion for HSV hepatitis and HSV encephalitis.
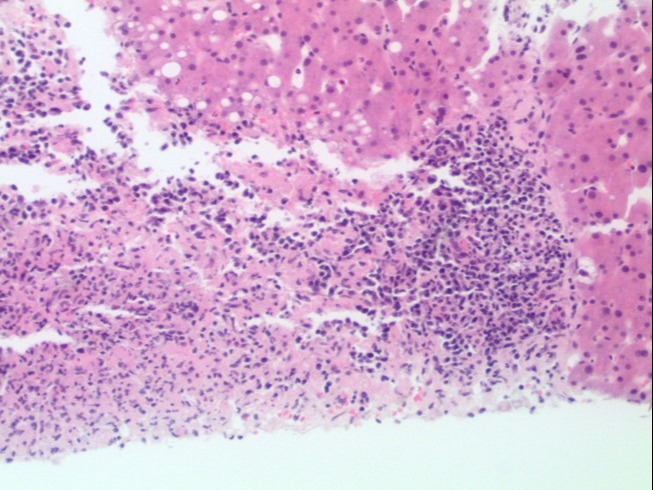
Ultimately, the cerebrospinal fluid studies demonstrated a positive HSV DNA. Liver biopsy demonstrated confluent liver necrosis involving the portal tract extending to Zone 2 with plasma cell predominance, and immunohistochemical staining was positive for HSV1 (Figure 1). Treatment was continued with improvement in the patient’s liver enzymes and mental status. Serial HSV quantitative serum PCRs were eventually undetectable. The patient recovered and was found to be at her baseline on outpatient follow-up.
Discussion: Patients who receive stem cell transplantation are considered immunocompromised for up to six weeks post-transplant and are at a higher risk of infection for one year. During this period, dormant viral infections such as HSV and VZV can be reactivated. This patient was immunocompromised, putting her at risk for reactivation of HSV. HSV hepatitis is an uncommon presentation of HSV that can cause fulminant hepatic failure in immunocompromised patients. Definitive diagnosis of HSV hepatitis can often delay diagnosis and increase mortality. Providers should maintain a high clinical suspicion for HSV hepatitis in immunocompromised patients presenting with acute liver failure and maintain a low threshold for starting anti-viral therapy if clinically indicated.
Disclosures:
Yara Dababneh, MD1, Aroob Sweidan, MD1, Poornima Oruganti, MD1, Syed-Mohammed Jafri, MD2, Qing Chang, MD1. B0566 - Be Suspicious: A Unique Case of Herpes Simplex Virus Hepatitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Henry Ford Hospital, Detroit, MI; 2Henry Ford Health System, Detroit, MI
Introduction: We present a case of disseminated HSV infection leading to acute liver failure and encephalitis in the setting of a history of autologous stem cell transplant.
Case Description/Methods: A 66-year-old female with a past medical history of amyloidosis status post chemotherapy and autologous stem cell transplant in 2018 and chronic kidney disease was transferred to a tertiary care facility for concern of acute liver failure. On initial presentation, she was encephalopathic. Laboratories demonstrated an AST of 5264 IU/L, ALT of 3237 IU/L, INR of 3.1, and creatinine of 5.92. No other significant personal or family history was found. Workup was negative for toxins.
The patient was considered immunocompromised. Her infectious workup was initially positive for E. coli in urine culture and Fusarium species in respiratory culture. The patient was initially thought to have liver hypoperfusion in the setting of severe sepsis. Serum testing for HSV1 and HSV2 was performed, and the HSV1 qualitative PCR was found to be positive. The patient’s liver enzymes remained elevated. Lumbar puncture was performed, and the patient was initiated on intravenous Acyclovir given a high index of suspicion for HSV hepatitis and HSV encephalitis.
Ultimately, the cerebrospinal fluid studies demonstrated a positive HSV DNA. Liver biopsy demonstrated confluent liver necrosis involving the portal tract extending to Zone 2 with plasma cell predominance, and immunohistochemical staining was positive for HSV1 (Figure 1). Treatment was continued with improvement in the patient’s liver enzymes and mental status. Serial HSV quantitative serum PCRs were eventually undetectable. The patient recovered and was found to be at her baseline on outpatient follow-up.
Discussion: Patients who receive stem cell transplantation are considered immunocompromised for up to six weeks post-transplant and are at a higher risk of infection for one year. During this period, dormant viral infections such as HSV and VZV can be reactivated. This patient was immunocompromised, putting her at risk for reactivation of HSV. HSV hepatitis is an uncommon presentation of HSV that can cause fulminant hepatic failure in immunocompromised patients. Definitive diagnosis of HSV hepatitis can often delay diagnosis and increase mortality. Providers should maintain a high clinical suspicion for HSV hepatitis in immunocompromised patients presenting with acute liver failure and maintain a low threshold for starting anti-viral therapy if clinically indicated.
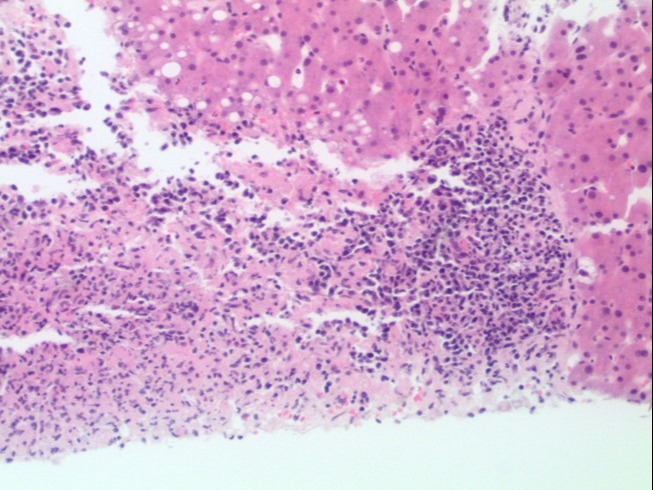
Figure: Figure 1: H&E stain of liver biopsy showing confluent liver necrosis involving the portal tract and extending to Zone 2. A moderate inflammatory infiltrate with plasma cell predominance located at the periphery of the necrotic area. No interface hepatitis or lobular inflammation is identified. Rare hepatocyte nuclei show smudge chromatin pattern, suggestive of a viral cytopathic effect.
Disclosures:
Yara Dababneh indicated no relevant financial relationships.
Aroob Sweidan indicated no relevant financial relationships.
Poornima Oruganti indicated no relevant financial relationships.
Syed-Mohammed Jafri indicated no relevant financial relationships.
Qing Chang indicated no relevant financial relationships.
Yara Dababneh, MD1, Aroob Sweidan, MD1, Poornima Oruganti, MD1, Syed-Mohammed Jafri, MD2, Qing Chang, MD1. B0566 - Be Suspicious: A Unique Case of Herpes Simplex Virus Hepatitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
