Back

Poster Session B - Monday Morning
Category: GI Bleeding
B0327 - Life Threatening Upper GI Bleed from Gastrosplenic Fistula: A Rare Complication of Splenic Diffuse Large B-Cell Lymphoma
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- SP
Syed Bilal Pasha, MD
University of Missouri
Columbia, MO
Presenting Author(s)
Hamza Ertugrul, MD1, Syed Bilal Pasha, MD1, Harleen K. Chela, MD2, Hakeem Akanbi, MD1, Tahan Veysel, MD1, Ebubekir Daglilar, MD1
1University of Missouri, Columbia, MO; 2University of Missouri-Columbia, Columbia, MO
Introduction: Gastrosplenic fistula (GSF) is a rare complication of splenic Diffuse Large B Cell Lymphoma (DLBCL) which, within itself, is a rare condition. The paucity of data makes early recognition, and management of complications such as life-threatening GI bleed, a challenge. Herein, we discuss a case of GSF presenting with acute, life-threatening GI bleed that was difficult to control, highlighting the challenges of management and diagnosis.
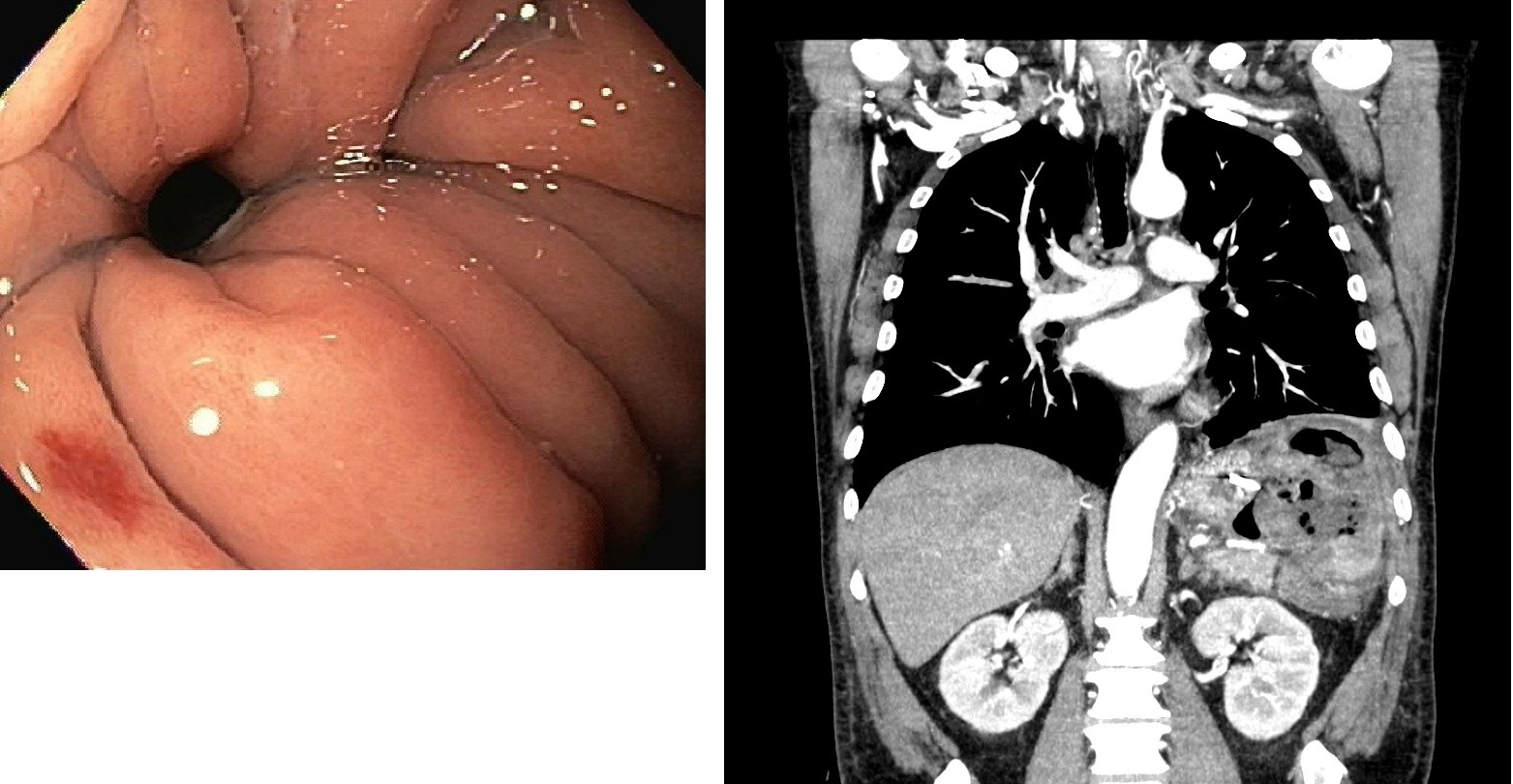
Case Description/Methods: A 56-year-old male was brought to a local hospital in critical condition due to a massive upper GI bleed after undergoing 2 cycles of R-CHOP chemotherapy for recently diagnosed DLBCL. Urgent upper endoscopy demonstrated a necrotic base ulcer in the fundus with active bleeding, and endoscopic interventions were inadequate in achieving hemostasis. Subsequent CT angiogram showed GSF with active bleeding from a branch of gastrosplenic artery. Splenic artery embolization was performed and patient was transferred to our institution for further care.
Patient continued to required blood transfusions without overt bleeding and repeat CT revealed a large splenic air and fluid collection, contiguous with stomach along with a focal deficit in the posterior gastric wall. Second look endoscopy was performed, which showed a large fistula in the fundus. Surgical oncology was consulted and by this time his GI bleeding had resolved. It was decided to proceed with conservative management, with follow-up imaging and he was subsequently discharged home in a stable condition.
Discussion: DLBCL is an aggressive and invasive type of lymphoma. The spread to local organs such as the stomach can cause fistula formation both spontaneously or due to rapid tumor cell death and necrosis from chemotherapy which is the probable underlying mechanism in our case. GI bleeding from GSF is very rare, and the life-threatening nature and difficulty in achieving endoscopic hemostasis makes them a challenge for gastroenterologists. Timely diagnosis is critical for management and the best modality appears to be CT, which is superior to EGD. The visualization of the fistula tract itself can be the best diagnostic clue, but this can often be difficult, so having high suspicion in the right clinical context is very important.
Preoperative splenic artery embolization has also been employed to stabilize patients with massive bleeding. Definitive treatment revolves around surgery, which includes open splenectomy with partial gastrectomy. Selected cases can be managed without surgery.
Disclosures:
Hamza Ertugrul, MD1, Syed Bilal Pasha, MD1, Harleen K. Chela, MD2, Hakeem Akanbi, MD1, Tahan Veysel, MD1, Ebubekir Daglilar, MD1. B0327 - Life Threatening Upper GI Bleed from Gastrosplenic Fistula: A Rare Complication of Splenic Diffuse Large B-Cell Lymphoma, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Missouri, Columbia, MO; 2University of Missouri-Columbia, Columbia, MO
Introduction: Gastrosplenic fistula (GSF) is a rare complication of splenic Diffuse Large B Cell Lymphoma (DLBCL) which, within itself, is a rare condition. The paucity of data makes early recognition, and management of complications such as life-threatening GI bleed, a challenge. Herein, we discuss a case of GSF presenting with acute, life-threatening GI bleed that was difficult to control, highlighting the challenges of management and diagnosis.
Case Description/Methods: A 56-year-old male was brought to a local hospital in critical condition due to a massive upper GI bleed after undergoing 2 cycles of R-CHOP chemotherapy for recently diagnosed DLBCL. Urgent upper endoscopy demonstrated a necrotic base ulcer in the fundus with active bleeding, and endoscopic interventions were inadequate in achieving hemostasis. Subsequent CT angiogram showed GSF with active bleeding from a branch of gastrosplenic artery. Splenic artery embolization was performed and patient was transferred to our institution for further care.
Patient continued to required blood transfusions without overt bleeding and repeat CT revealed a large splenic air and fluid collection, contiguous with stomach along with a focal deficit in the posterior gastric wall. Second look endoscopy was performed, which showed a large fistula in the fundus. Surgical oncology was consulted and by this time his GI bleeding had resolved. It was decided to proceed with conservative management, with follow-up imaging and he was subsequently discharged home in a stable condition.
Discussion: DLBCL is an aggressive and invasive type of lymphoma. The spread to local organs such as the stomach can cause fistula formation both spontaneously or due to rapid tumor cell death and necrosis from chemotherapy which is the probable underlying mechanism in our case. GI bleeding from GSF is very rare, and the life-threatening nature and difficulty in achieving endoscopic hemostasis makes them a challenge for gastroenterologists. Timely diagnosis is critical for management and the best modality appears to be CT, which is superior to EGD. The visualization of the fistula tract itself can be the best diagnostic clue, but this can often be difficult, so having high suspicion in the right clinical context is very important.
Preoperative splenic artery embolization has also been employed to stabilize patients with massive bleeding. Definitive treatment revolves around surgery, which includes open splenectomy with partial gastrectomy. Selected cases can be managed without surgery.
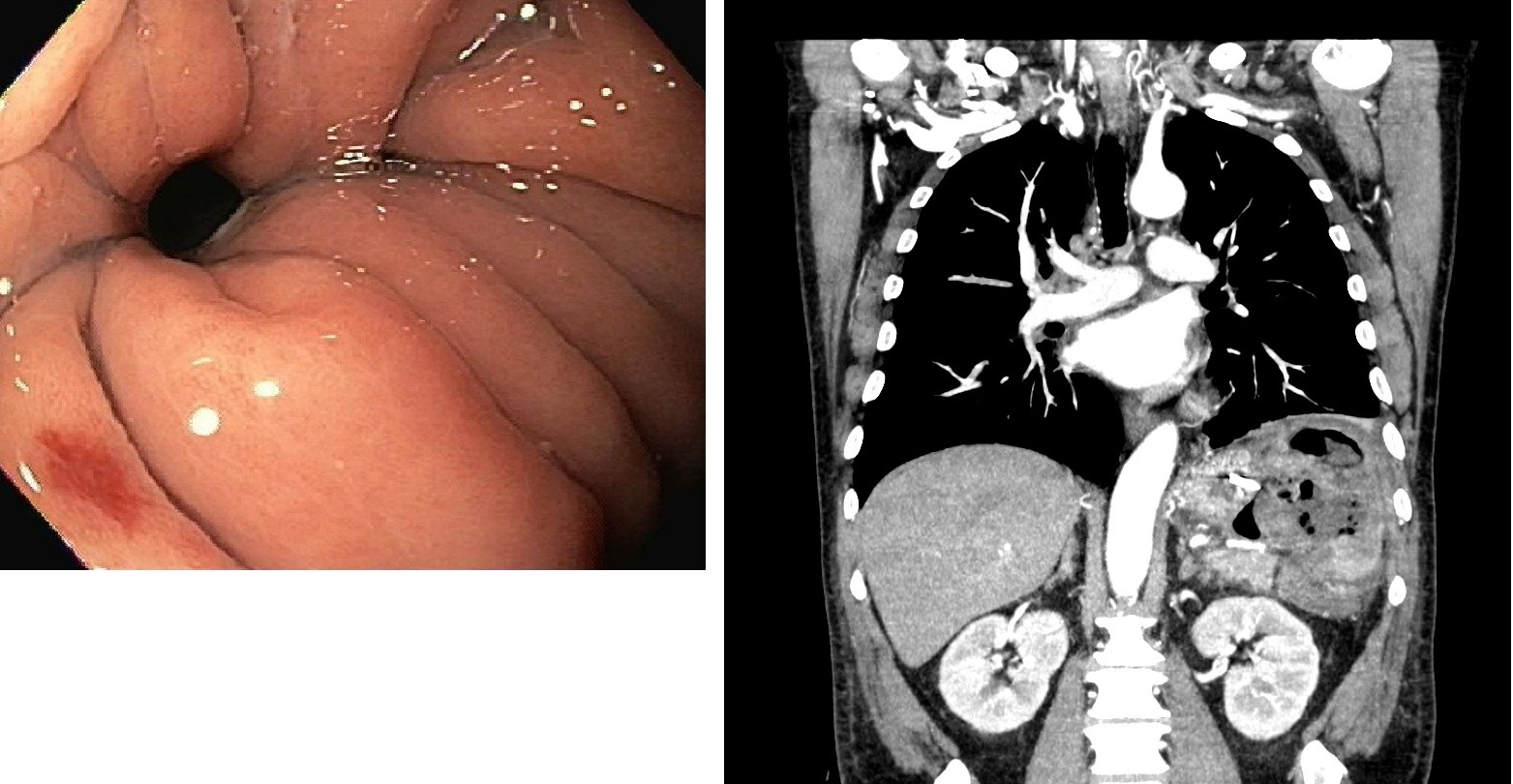
Figure: EGD showing fistula in gastric fundus
Fistulous tract and splenic fluid/air collection seen on abdominal CT
Fistulous tract and splenic fluid/air collection seen on abdominal CT
Disclosures:
Hamza Ertugrul indicated no relevant financial relationships.
Syed Bilal Pasha indicated no relevant financial relationships.
Harleen Chela indicated no relevant financial relationships.
Hakeem Akanbi indicated no relevant financial relationships.
Tahan Veysel indicated no relevant financial relationships.
Tahan Veysel — NO DISCLOSURE DATA.
Ebubekir Daglilar indicated no relevant financial relationships.
Hamza Ertugrul, MD1, Syed Bilal Pasha, MD1, Harleen K. Chela, MD2, Hakeem Akanbi, MD1, Tahan Veysel, MD1, Ebubekir Daglilar, MD1. B0327 - Life Threatening Upper GI Bleed from Gastrosplenic Fistula: A Rare Complication of Splenic Diffuse Large B-Cell Lymphoma, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
