Back

Poster Session A - Sunday Afternoon
Category: Small Intestine
A0651 - A Case of Systemic Mastocytosis Diagnosed Endoscopically
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Ariana R. Tagliaferri, MD
Saint Joseph's University Medical Center
Paterson, NJ
Presenting Author(s)
Award: Presidential Poster Award
Ariana R. Tagliaferri, MD1, Devina Adalja, MD2, Yana Cavanagh, MD1
1Saint Joseph's University Medical Center, Paterson, NJ; 2St. Joseph's Regional Medical Center, Paterson, NJ
Introduction: Mastocytosis, or mast cell proliferation has an annual incidence of 2/100,000. Only 10% of all Mastocytosis is considered systemic (SM); the most common site of involvement is the bone marrow, however of those ~60% will also have gastrointestinal symptoms. The colon is often affected most and endoscopically, there is mucosal nodularity, loss of normal architecture and friability with pathologically positive dense mast cell infiltration of the lamina propria. Indolent SM is characterized by both gastrointestinal and cutaneous symptoms, in the absence of bone marrow suppression and end-organ damage. It is extremely rare and often missed due to the complexity of diagnosis. We present a patient with abdominal pain, flushing and nausea who was diagnosed endoscopically with Systemic Mastocytosis, likely indolent type.
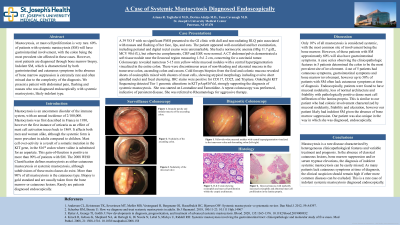
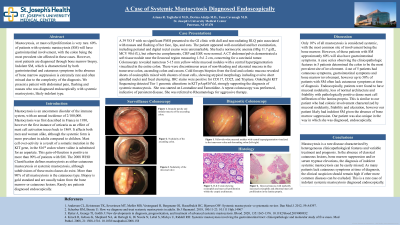
Case Description/Methods: A 39 YO F with no significant PMH presented to the GI clinic with dull and non-radiating RLQ pain associated with nausea and flushing of her face, lips, and ears. The patient appeared well-nourished and her examination, including perianal and digital rectal exams were unremarkable. She had a normocytic anemia (Hbg 11.7 g/dL, MCV 90.6 fL), but otherwise complements, CRP and ESR were normal. A CT abdomen/pelvis demonstrated a soft tissue nodule near the ileocecal region measuring 1.5x1.2 cm, concerning for a carcinoid tumor. Colonoscopy revealed numerous 5-15 mm yellow-white mucosal nodules with central hyperpigmentation visualized in the entire colon. There were discontinuous areas of non-bleeding and ulcerated mucosa in the transverse colon, ascending colon and cecum. Cold forceps biopsies from the ileal and colonic mucosa revealed sheets of eosinophils mixed with clusters of mast cells, showing atypical morphology including oval to short-spindled nuclei and focal clustering. IHC stains were positive for CD117, CD25, and Tryptase. OnkoSight KIT Sequencing detected Tier 1 genomic alterations in KIT pAsp816Val, strongly supporting the diagnosis of Systemic Mastocytosis. She was referred to Rheumatology for further workup.
Discussion: Mastocytosis is a rare disease characterized by heterogeneous clinicopathological features. In the absence of classical cutaneous lesions, bone marrow suppression and/or serum tryptase elevations, the diagnosis of Indolent Systemic Mastocytosis can be easily missed. As many patients lack cutaneous symptoms at time of diagnosis, the clinical suspicion should remain high if other more common diseases can be excluded.
Disclosures:
Ariana R. Tagliaferri, MD1, Devina Adalja, MD2, Yana Cavanagh, MD1. A0651 - A Case of Systemic Mastocytosis Diagnosed Endoscopically, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Ariana R. Tagliaferri, MD1, Devina Adalja, MD2, Yana Cavanagh, MD1
1Saint Joseph's University Medical Center, Paterson, NJ; 2St. Joseph's Regional Medical Center, Paterson, NJ
Introduction: Mastocytosis, or mast cell proliferation has an annual incidence of 2/100,000. Only 10% of all Mastocytosis is considered systemic (SM); the most common site of involvement is the bone marrow, however of those ~60% will also have gastrointestinal symptoms. The colon is often affected most and endoscopically, there is mucosal nodularity, loss of normal architecture and friability with pathologically positive dense mast cell infiltration of the lamina propria. Indolent SM is characterized by both gastrointestinal and cutaneous symptoms, in the absence of bone marrow suppression and end-organ damage. It is extremely rare and often missed due to the complexity of diagnosis. We present a patient with abdominal pain, flushing and nausea who was diagnosed endoscopically with Systemic Mastocytosis, likely indolent type.
Case Description/Methods: A 39 YO F with no significant PMH presented to the GI clinic with dull and non-radiating RLQ pain associated with nausea and flushing of her face, lips, and ears. The patient appeared well-nourished and her examination, including perianal and digital rectal exams were unremarkable. She had a normocytic anemia (Hbg 11.7 g/dL, MCV 90.6 fL), but otherwise complements, CRP and ESR were normal. A CT abdomen/pelvis demonstrated a soft tissue nodule near the ileocecal region measuring 1.5x1.2 cm, concerning for a carcinoid tumor. Colonoscopy revealed numerous 5-15 mm yellow-white mucosal nodules with central hyperpigmentation visualized in the entire colon. There were discontinuous areas of non-bleeding and ulcerated mucosa in the transverse colon, ascending colon and cecum. Cold forceps biopsies from the ileal and colonic mucosa revealed sheets of eosinophils mixed with clusters of mast cells, showing atypical morphology including oval to short-spindled nuclei and focal clustering. IHC stains were positive for CD117, CD25, and Tryptase. OnkoSight KIT Sequencing detected Tier 1 genomic alterations in KIT pAsp816Val, strongly supporting the diagnosis of Systemic Mastocytosis. She was referred to Rheumatology for further workup.
Discussion: Mastocytosis is a rare disease characterized by heterogeneous clinicopathological features. In the absence of classical cutaneous lesions, bone marrow suppression and/or serum tryptase elevations, the diagnosis of Indolent Systemic Mastocytosis can be easily missed. As many patients lack cutaneous symptoms at time of diagnosis, the clinical suspicion should remain high if other more common diseases can be excluded.
Disclosures:
Ariana Tagliaferri indicated no relevant financial relationships.
Devina Adalja indicated no relevant financial relationships.
Yana Cavanagh indicated no relevant financial relationships.
Ariana R. Tagliaferri, MD1, Devina Adalja, MD2, Yana Cavanagh, MD1. A0651 - A Case of Systemic Mastocytosis Diagnosed Endoscopically, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.


