Back

Poster Session C - Monday Afternoon
Category: Colon
C0127 - Anorectal Melanoma
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Khaled Elfert, MD, MRCP
SBH Health System
New York, NY
Presenting Author(s)
Mahmoud Elgawish, MD1, Ahmad Aboelezz, MBChB, MS1, Ahmed Metawee, MD1, Mouhand F. Mohamed, MD, MSc2, Khaled Elfert, MD, MRCP3
1Tanta University Hospitals, Tanta, Al Gharbiyah, Egypt; 2Warren Alpert Medical School of Brown University, Providence, RI; 3SBH Health System, New York, NY
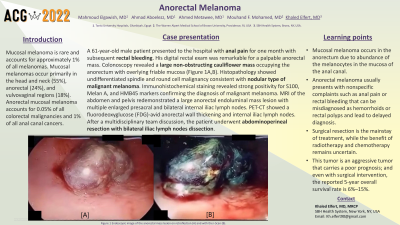
Introduction: Mucosal melanoma is rare and accounts for approximately 1% of all melanomas. Mucosal melanomas occur primarily in the head and neck (55%), anorectal, and vulvovaginal regions (18%). Anorectal mucosal melanoma accounts for 0.05% of all colorectal malignancies and 1% of all anal canal cancers.
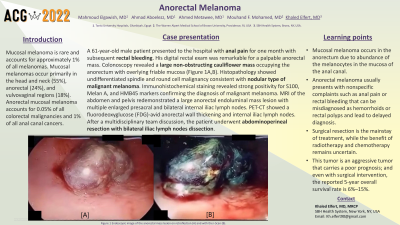
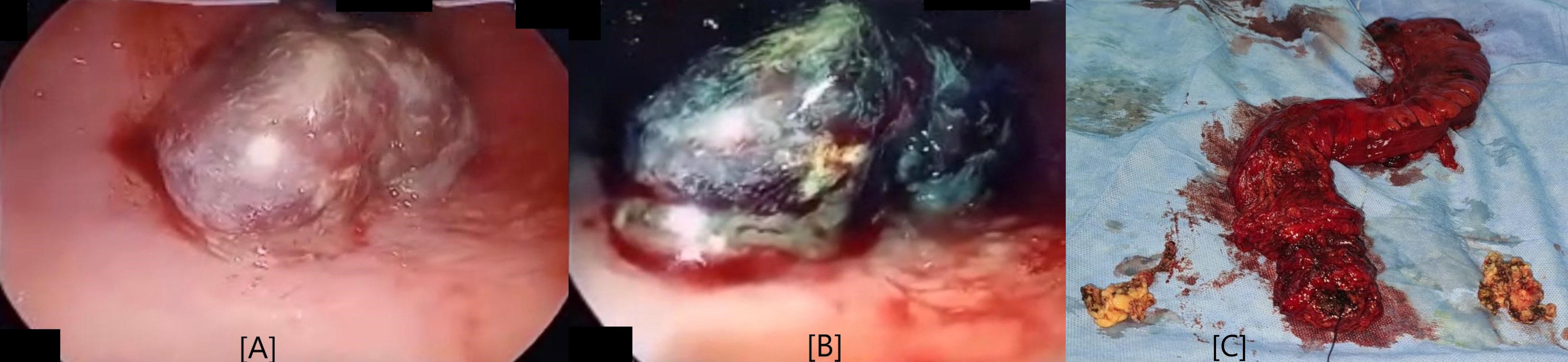
Case Description/Methods: A 61 year-old-male patient with no significant past medical history presented to the hospital with anal pain for one month with subsequent rectal bleeding. On examination, his heart rate and blood pressure were within normal limits. His digital rectal exam was remarkable for a palpable anorectal mass. His blood tests showed no anemia. Colonoscopy revealed a large non-obstructing cauliflower mass occupying the anorectum with overlying friable mucosa that easily bleeds on touch (Figure 1a,b). Histopathology showed undifferentiated spindle and round cell malignancy consistent with nodular type of malignant melanoma. Immunohistochemical staining revealed strong positivity for S100, Melan A, and HMB45 markers confirming the diagnosis of malignant melanoma. Magnetic resonance imaging (MRI) of the abdomen and pelvis redemonstrated a large anorectal endoluminal mass lesion with multiple enlarged presacral and bilateral internal iliac lymph nodes. Positron emission tomography-computed tomography scan (PET-CT) showed a fluorodeoxyglucose (FDG)-avid anorectal wall thickening and internal iliac lymph nodes. After a multidisciplinary team discussion, the patient underwent abdominoperineal resection with bilateral iliac lymph nodes dissection (Figure 1c).
Discussion: Malignant melanoma of the anorectum is a rare mucosal neoplasm that typically presents in the fifth or sixth decade. Mucosal melanoma occurs in the anorectum due to abundance of the melanocytes in the mucosa of the anal canal. It usually presents with nonspecific complaints such as anal pain or rectal bleeding that can be misdiagnosed as hemorrhoids or rectal polyps and lead to delayed diagnosis. Surgical resection is the mainstay of treatment, while the benefit of radiotherapy and chemotherapy remains uncertain. This tumor is an aggressive tumor that carries a poor prognosis; and even with surgical intervention, the reported 5-year overall survival rate is 6%–15%.
Disclosures:
Mahmoud Elgawish, MD1, Ahmad Aboelezz, MBChB, MS1, Ahmed Metawee, MD1, Mouhand F. Mohamed, MD, MSc2, Khaled Elfert, MD, MRCP3. C0127 - Anorectal Melanoma, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Tanta University Hospitals, Tanta, Al Gharbiyah, Egypt; 2Warren Alpert Medical School of Brown University, Providence, RI; 3SBH Health System, New York, NY
Introduction: Mucosal melanoma is rare and accounts for approximately 1% of all melanomas. Mucosal melanomas occur primarily in the head and neck (55%), anorectal, and vulvovaginal regions (18%). Anorectal mucosal melanoma accounts for 0.05% of all colorectal malignancies and 1% of all anal canal cancers.
Case Description/Methods: A 61 year-old-male patient with no significant past medical history presented to the hospital with anal pain for one month with subsequent rectal bleeding. On examination, his heart rate and blood pressure were within normal limits. His digital rectal exam was remarkable for a palpable anorectal mass. His blood tests showed no anemia. Colonoscopy revealed a large non-obstructing cauliflower mass occupying the anorectum with overlying friable mucosa that easily bleeds on touch (Figure 1a,b). Histopathology showed undifferentiated spindle and round cell malignancy consistent with nodular type of malignant melanoma. Immunohistochemical staining revealed strong positivity for S100, Melan A, and HMB45 markers confirming the diagnosis of malignant melanoma. Magnetic resonance imaging (MRI) of the abdomen and pelvis redemonstrated a large anorectal endoluminal mass lesion with multiple enlarged presacral and bilateral internal iliac lymph nodes. Positron emission tomography-computed tomography scan (PET-CT) showed a fluorodeoxyglucose (FDG)-avid anorectal wall thickening and internal iliac lymph nodes. After a multidisciplinary team discussion, the patient underwent abdominoperineal resection with bilateral iliac lymph nodes dissection (Figure 1c).
Discussion: Malignant melanoma of the anorectum is a rare mucosal neoplasm that typically presents in the fifth or sixth decade. Mucosal melanoma occurs in the anorectum due to abundance of the melanocytes in the mucosa of the anal canal. It usually presents with nonspecific complaints such as anal pain or rectal bleeding that can be misdiagnosed as hemorrhoids or rectal polyps and lead to delayed diagnosis. Surgical resection is the mainstay of treatment, while the benefit of radiotherapy and chemotherapy remains uncertain. This tumor is an aggressive tumor that carries a poor prognosis; and even with surgical intervention, the reported 5-year overall survival rate is 6%–15%.
Figure: Endoscopic image of the anorectal mass lesion on retroflection (A) and with the i-Scan (B).
(C) Abdominoperineal resection with bilateral iliac lymph nodes dissection.
(C) Abdominoperineal resection with bilateral iliac lymph nodes dissection.
Disclosures:
Mahmoud Elgawish indicated no relevant financial relationships.
Ahmad Aboelezz indicated no relevant financial relationships.
Ahmed Metawee indicated no relevant financial relationships.
Mouhand Mohamed indicated no relevant financial relationships.
Khaled Elfert indicated no relevant financial relationships.
Mahmoud Elgawish, MD1, Ahmad Aboelezz, MBChB, MS1, Ahmed Metawee, MD1, Mouhand F. Mohamed, MD, MSc2, Khaled Elfert, MD, MRCP3. C0127 - Anorectal Melanoma, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
