Back

Poster Session C - Monday Afternoon
Category: IBD
C0433 - Rituxan-Induced Colitis
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio
- MM
Maryam Mubashir, MD
Louisiana State University Health Sciences Center
Shreveport, LA
Presenting Author(s)
Maryam Mubashir, MD1, Fatima Hassan, MD1, Aditya Vyas, MD2, Muhammad Saad Ahmad, MBBS1, Hassaan Zia, MD1
1O-LSUS, Shreveport, LA; 2Louisiana State University Health Sciences Center, Shreveport, LA
Introduction: Rituximab is a monoclonal antibody which is increasingly being used to treat autoimmune disorders and certain cancers. With this, we are also coming across Gastrointestinal toxicities. These are, however, usually self limited diarrhea and abdominal pain requiring supportive management. We present a case of a patient who developed Crohn’s disease after use of Rituximab requiring long term immunosuppressive therapy.
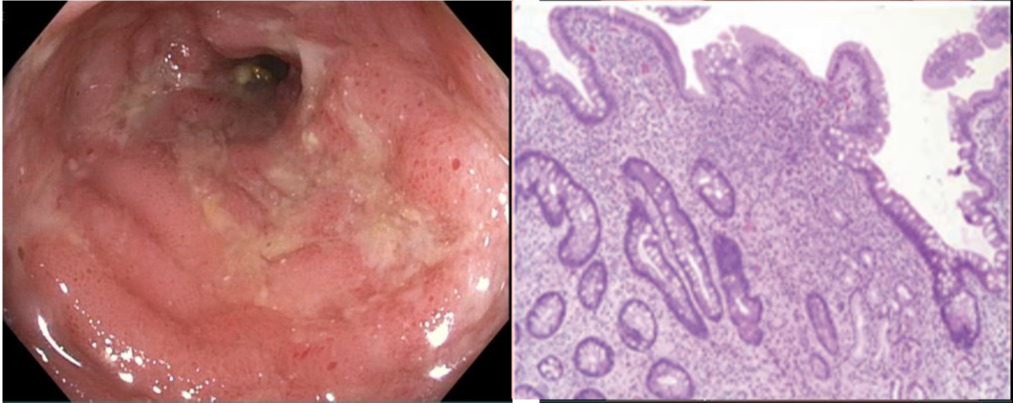
Case Description/Methods: 67-year-old lady came in with 6 months of generalized lower abdominal pain and 7-9 episodes of watery diarrhea, along with unintentional weight loss. She had a history of well controlled Rheumatoid Arthritis/ Mixed connective tissue disease on Rituximab, failing multiple therapies in the past. CT abdomen showed Mural thickening in Terminal ileum, Cecum, and Ascending colon with enteric lymphadenopathies. The patient underwent colonoscopy for further evaluation which showed Ulceration, erythema and friable mucosa in terminal Ileum. The rest of the examined colon appeared normal. Pathology showed severe active ileitis and mild active colitis in transverse colon, while rest of segments were normal. Rituximab was stopped as a therapeutic trial which significantly improved the patient's symptoms. Her CDAI score improved from 289 points to 177 points. However Inflammatory markers, Imaging and endoscopic disease, despite improving, did not resolve completely. Ustekinumab was started after extensive discussion. After 6 months she had a complete clinical, endoscopic and histopathologic remission.
Discussion: Gastrointestinal toxicities of Rituximab are a well-known entity. The exact pathophysiology of rituximab induced colitis however, remains unclear. B and T lymphocytes interact in the intestinal wall and are responsible for mucosal immunoregulation, which increases immune tolerance. With Rituximab induced depletion of CD20+ B cells there is an increase infiltration of T lymphocytes in the intestinal mucosa which can potentially cause an immunogenic response resulting in IBD like colitis. A rare disease, drug induced IBD is mild uncomplicated and short lived requiring only supportive management and discontinuation of offending agent. Only a few cases are reported where patient fails to improve and require Immunosuppressive therapy. More data is needed on how to differentiate between primary vs drug induced IBD in addition to finding the ideal agent to treat drug induced IBD and long term outcomes of this disease sub set.
Disclosures:
Maryam Mubashir, MD1, Fatima Hassan, MD1, Aditya Vyas, MD2, Muhammad Saad Ahmad, MBBS1, Hassaan Zia, MD1. C0433 - Rituxan-Induced Colitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1O-LSUS, Shreveport, LA; 2Louisiana State University Health Sciences Center, Shreveport, LA
Introduction: Rituximab is a monoclonal antibody which is increasingly being used to treat autoimmune disorders and certain cancers. With this, we are also coming across Gastrointestinal toxicities. These are, however, usually self limited diarrhea and abdominal pain requiring supportive management. We present a case of a patient who developed Crohn’s disease after use of Rituximab requiring long term immunosuppressive therapy.
Case Description/Methods: 67-year-old lady came in with 6 months of generalized lower abdominal pain and 7-9 episodes of watery diarrhea, along with unintentional weight loss. She had a history of well controlled Rheumatoid Arthritis/ Mixed connective tissue disease on Rituximab, failing multiple therapies in the past. CT abdomen showed Mural thickening in Terminal ileum, Cecum, and Ascending colon with enteric lymphadenopathies. The patient underwent colonoscopy for further evaluation which showed Ulceration, erythema and friable mucosa in terminal Ileum. The rest of the examined colon appeared normal. Pathology showed severe active ileitis and mild active colitis in transverse colon, while rest of segments were normal. Rituximab was stopped as a therapeutic trial which significantly improved the patient's symptoms. Her CDAI score improved from 289 points to 177 points. However Inflammatory markers, Imaging and endoscopic disease, despite improving, did not resolve completely. Ustekinumab was started after extensive discussion. After 6 months she had a complete clinical, endoscopic and histopathologic remission.
Discussion: Gastrointestinal toxicities of Rituximab are a well-known entity. The exact pathophysiology of rituximab induced colitis however, remains unclear. B and T lymphocytes interact in the intestinal wall and are responsible for mucosal immunoregulation, which increases immune tolerance. With Rituximab induced depletion of CD20+ B cells there is an increase infiltration of T lymphocytes in the intestinal mucosa which can potentially cause an immunogenic response resulting in IBD like colitis. A rare disease, drug induced IBD is mild uncomplicated and short lived requiring only supportive management and discontinuation of offending agent. Only a few cases are reported where patient fails to improve and require Immunosuppressive therapy. More data is needed on how to differentiate between primary vs drug induced IBD in addition to finding the ideal agent to treat drug induced IBD and long term outcomes of this disease sub set.
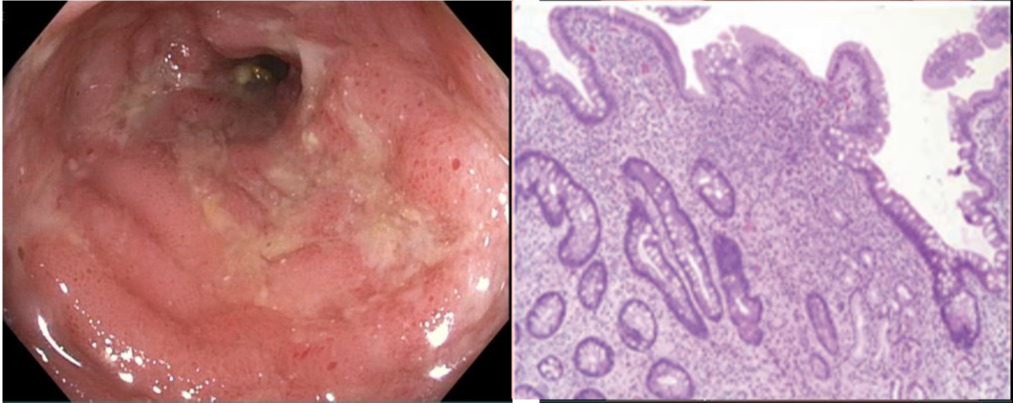
Figure: Ulceration/inflammation in terminal Ileum
Disclosures:
Maryam Mubashir indicated no relevant financial relationships.
Fatima Hassan indicated no relevant financial relationships.
Aditya Vyas indicated no relevant financial relationships.
Muhammad Saad Ahmad indicated no relevant financial relationships.
Hassaan Zia indicated no relevant financial relationships.
Maryam Mubashir, MD1, Fatima Hassan, MD1, Aditya Vyas, MD2, Muhammad Saad Ahmad, MBBS1, Hassaan Zia, MD1. C0433 - Rituxan-Induced Colitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

