Back

Poster Session A - Sunday Afternoon
Category: Esophagus
A0224 - Esophageal Perforation Following Atrial Fibrillation Ablation: A Review of Ablation-Associated Esophageal Injury
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Julianna Tantum, DO
Lankenau Medical Center
Wynnewood, PA
Presenting Author(s)
Award: Presidential Poster Award
Julianna Tantum, DO1, Amanda Long, DO1, Patricia Wong, MD2
1Lankenau Medical Center, Wynnewood, PA; 2Lankenau Medical Center, Philadelphia, PA
Introduction: Catheter ablation is a common treatment for refractory atrial fibrillation (AF). Due to the close proximity of the esophagus to the left atrium, there is risk for esophageal injury, some of which have high morbidity. We present a case of a patient who developed an esophageal perforation, pulmonary vein thrombosis, and embolic stroke one month after AF ablation.
Case Description/Methods:
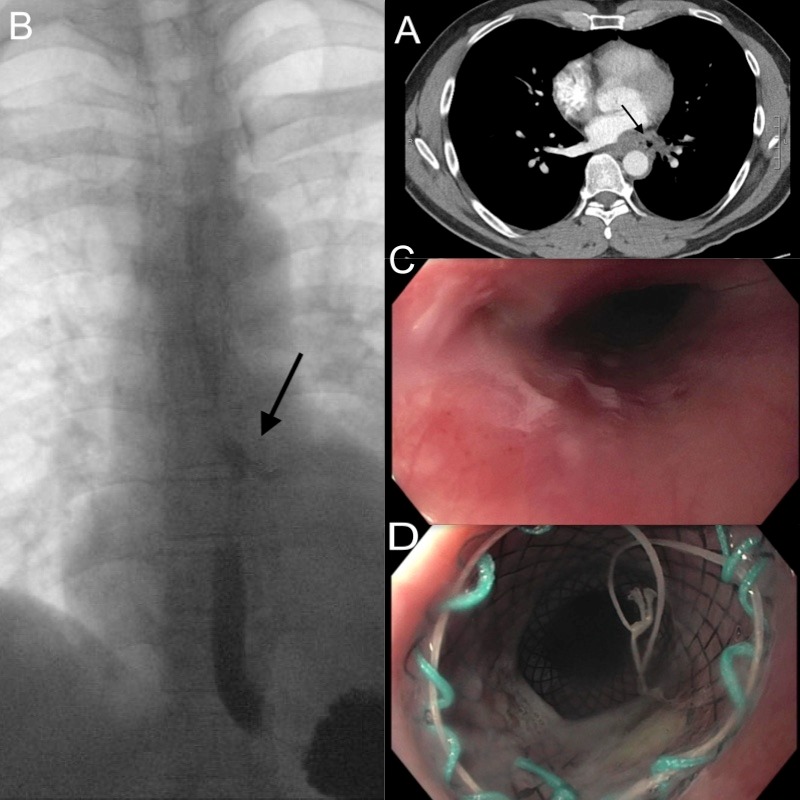
A 49-year-old male with a history of AF presented to the hospital with heartburn, dysphagia, fevers and interscapular pain one month after AF ablation. On exam he was febrile to 103.3F, abdominal exam was benign and no crepitus was appreciated. Labs showed WBC 10.9 K/uL. CT chest with IV contrast showed thickening in the posterior wall of the left atrium and small air pockets in the left infrahilar region (Image 1A). Blood cultures were obtained, and later grew Streptococcus mitis.
On hospital day 2, he developed left upper extremity weakness. Brain MRI showed small embolic infarcts. TEE was attempted but incomplete due to resistance in the proximal esophagus. Gastrograffin swallow study showed extravasation of contrast from the esophagus, consistent with an esophageal perforation (Image 1B). CTA chest showed hemorrhage in the left lower lobe (LLL) and venous congestion with occlusion of the left pulmonary vein. Esophagoscopy showed blood throughout the esophagus with a small mucosal defect with clot at 38 cm, without evidence of atrio esophageal fistula (AEF) (Image 1C). He underwent a left lower lobectomy. He was treated with ceftriaxone, vancomycin, and micafungin. After failed conservative therapy, a partially covered esophageal stent was placed (Image 1D). He was discharged on a 6-week course of ceftriaxone.
Discussion: As catheter AF ablation becomes increasingly common, it is important to recognize the potential for esophageal injury. Patients present 1 to 4 weeks post-ablation with chest pain, acid reflux, and dysphagia. Imaging of choice is CT with IV and oral contrast. Management depends on the extent of injury but ranges from endoscopic stent placement to open surgical intervention. Techniques to reduce the risk of injury include using an esophageal temperature probe and gastric suppression therapy. Esophageal injury may occur in about 47% of patients, including mild thermal burns, vagus nerve injury, perforation and AEF. This case outlines the importance of keeping esophageal pathology in the differential in patients who present with non-specific symptoms during the months following AF ablation.
Disclosures:
Julianna Tantum, DO1, Amanda Long, DO1, Patricia Wong, MD2. A0224 - Esophageal Perforation Following Atrial Fibrillation Ablation: A Review of Ablation-Associated Esophageal Injury, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Julianna Tantum, DO1, Amanda Long, DO1, Patricia Wong, MD2
1Lankenau Medical Center, Wynnewood, PA; 2Lankenau Medical Center, Philadelphia, PA
Introduction: Catheter ablation is a common treatment for refractory atrial fibrillation (AF). Due to the close proximity of the esophagus to the left atrium, there is risk for esophageal injury, some of which have high morbidity. We present a case of a patient who developed an esophageal perforation, pulmonary vein thrombosis, and embolic stroke one month after AF ablation.
Case Description/Methods:
A 49-year-old male with a history of AF presented to the hospital with heartburn, dysphagia, fevers and interscapular pain one month after AF ablation. On exam he was febrile to 103.3F, abdominal exam was benign and no crepitus was appreciated. Labs showed WBC 10.9 K/uL. CT chest with IV contrast showed thickening in the posterior wall of the left atrium and small air pockets in the left infrahilar region (Image 1A). Blood cultures were obtained, and later grew Streptococcus mitis.
On hospital day 2, he developed left upper extremity weakness. Brain MRI showed small embolic infarcts. TEE was attempted but incomplete due to resistance in the proximal esophagus. Gastrograffin swallow study showed extravasation of contrast from the esophagus, consistent with an esophageal perforation (Image 1B). CTA chest showed hemorrhage in the left lower lobe (LLL) and venous congestion with occlusion of the left pulmonary vein. Esophagoscopy showed blood throughout the esophagus with a small mucosal defect with clot at 38 cm, without evidence of atrio esophageal fistula (AEF) (Image 1C). He underwent a left lower lobectomy. He was treated with ceftriaxone, vancomycin, and micafungin. After failed conservative therapy, a partially covered esophageal stent was placed (Image 1D). He was discharged on a 6-week course of ceftriaxone.
Discussion: As catheter AF ablation becomes increasingly common, it is important to recognize the potential for esophageal injury. Patients present 1 to 4 weeks post-ablation with chest pain, acid reflux, and dysphagia. Imaging of choice is CT with IV and oral contrast. Management depends on the extent of injury but ranges from endoscopic stent placement to open surgical intervention. Techniques to reduce the risk of injury include using an esophageal temperature probe and gastric suppression therapy. Esophageal injury may occur in about 47% of patients, including mild thermal burns, vagus nerve injury, perforation and AEF. This case outlines the importance of keeping esophageal pathology in the differential in patients who present with non-specific symptoms during the months following AF ablation.
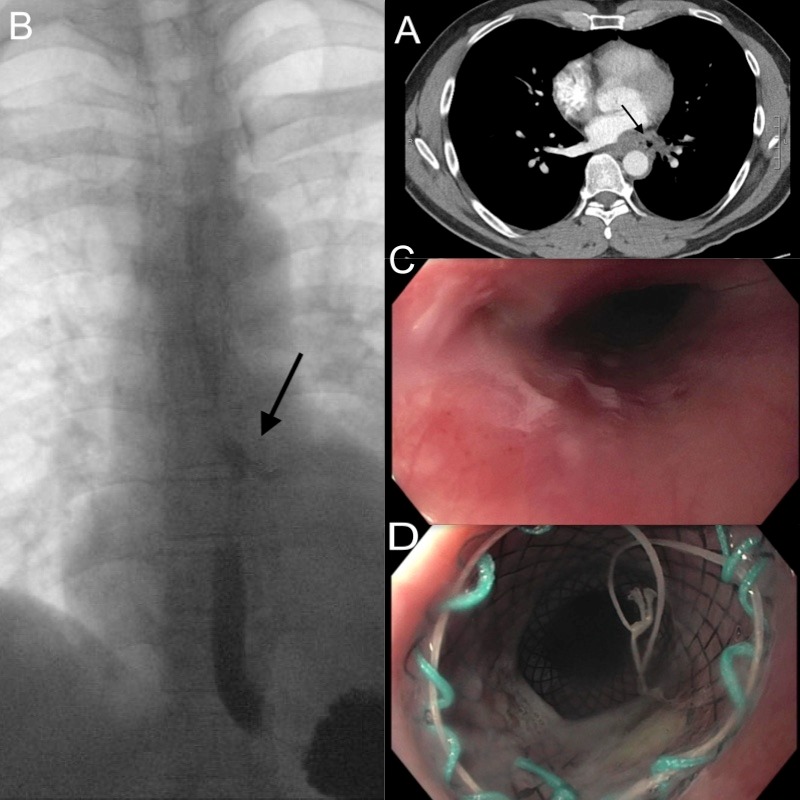
Figure: Image 1A. A computed tomography (CT) chest with intravenous contrast showing no evidence of an atrial-esophageal fistula but showed mild thickening in the left posterior aspect of the left atrium, also with tiny pockets of air in the left infrahilar region (arrow). Image 1B. Gastrograffin fluoroscopic swallow study showing evidence of an esophageal leak (arrow) 3cm below the left mainstem bronchus at the site of the tiny air pockets previously seen on CT imaging. Image 1C. Endoscopic imaging showing a small mucosal defect. Image 1D. Endoscopic imaging showing a partially covered esophageal stent.
Disclosures:
Julianna Tantum indicated no relevant financial relationships.
Amanda Long indicated no relevant financial relationships.
Patricia Wong indicated no relevant financial relationships.
Julianna Tantum, DO1, Amanda Long, DO1, Patricia Wong, MD2. A0224 - Esophageal Perforation Following Atrial Fibrillation Ablation: A Review of Ablation-Associated Esophageal Injury, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.


