Back

Poster Session B - Monday Morning
Category: Liver
B0613 - Acute Intermittent Porphyria
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- AL
Andrew E. Lee, MD
Tower Health
Reading, PA
Presenting Author(s)
Alexandra Scanameo, MS, MS1, Shefali Amin, DO, MSEd2, Andrew E. Lee, MD3, John F. Altomare, MD4
1Drexel University College of Medicine, Philadelphia, PA; 2Reading Tower Health, Reading, PA; 3Tower Health, Reading, PA; 4Reading Hospital/Tower Health/Digestive Disease Associates, Wyomissing, PA
Introduction: An 18 year old female with no past medical history presented with an episode of severe abdominal pain, associated with nausea and vomiting. She had intermittent episodes for the past 2 years, and attacks usually occurred 1 week before her menses.
She was previously seen by her PCP, who suspected she had celiac disease and was placed on a gluten-free diet without improvement. A few months ago, she was admitted the hospital for similar complaints, and underwent both an upper endoscopy as well as a colonoscopy, both of which were unremarkable. She was discharged from the hospital at that time with a presumptive diagnosis of IBS.
On this admission, she was hypertensive. Additional review of systems included intermittent tingling at her fingertips, which she noticed more frequently. Labs were notable for a sodium of 126 mmol/L. Imaging, including a CT of her abdomen/pelvis as well as an MR Enterography, were unremarkable. The young patient continued to have pain despite opiate analgesics, which prompted the search for more rare etiologies of abdominal pain.
Case Description/Methods: Her total porphyrins were 20.1mcg/L, and random urine porphyrins were extremely elevated. Her Porphobilinogen Deaminase (PBGD) level was diminished, and was found to have a PBGD mutation. She was diagnosed with Acute Intermittent Porphyria. She was treated with hemin infusions with mild improvement in her symptoms, and oral glucose loading at onset of symptoms. However, her symptoms eventually came back, and she was initiated on Givosiran.
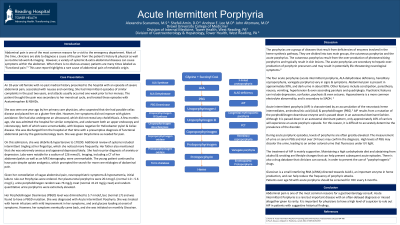
Discussion: Acute intermittent porphyria is an autosomal dominant condition with low penetrance of a mutation in the porphobilinogen deaminase (PBGD) gene, which leads to an accumulation of heme intermediates. Around 90% of carriers are asymptomatic, and thus, the prevalence is difficult to ascertain.
Abdominal pain is often the initial presenting symptom, and is characteristically severe & unremitting. It can be associated with other GI symptoms, including nausea, vomiting & diarrhea.
Neurologic symptoms, including peripheral neuropathy and muscle weakness can occur. Psychologic symptoms can also be present, including irritability, anxiety, paranoia & altered consciousness.
During an acute AIP attack, hyponatremia may also occur, and may lead to seizures.
The primary management of the disease revolves around prevention of attacks, including avoiding implicating medications, hormonal contraception, low-carb diets & alcohol. Pharmacologic therapy, including Givosiran, can also be used.
Disclosures:
Alexandra Scanameo, MS, MS1, Shefali Amin, DO, MSEd2, Andrew E. Lee, MD3, John F. Altomare, MD4. B0613 - Acute Intermittent Porphyria, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Drexel University College of Medicine, Philadelphia, PA; 2Reading Tower Health, Reading, PA; 3Tower Health, Reading, PA; 4Reading Hospital/Tower Health/Digestive Disease Associates, Wyomissing, PA
Introduction: An 18 year old female with no past medical history presented with an episode of severe abdominal pain, associated with nausea and vomiting. She had intermittent episodes for the past 2 years, and attacks usually occurred 1 week before her menses.
She was previously seen by her PCP, who suspected she had celiac disease and was placed on a gluten-free diet without improvement. A few months ago, she was admitted the hospital for similar complaints, and underwent both an upper endoscopy as well as a colonoscopy, both of which were unremarkable. She was discharged from the hospital at that time with a presumptive diagnosis of IBS.
On this admission, she was hypertensive. Additional review of systems included intermittent tingling at her fingertips, which she noticed more frequently. Labs were notable for a sodium of 126 mmol/L. Imaging, including a CT of her abdomen/pelvis as well as an MR Enterography, were unremarkable. The young patient continued to have pain despite opiate analgesics, which prompted the search for more rare etiologies of abdominal pain.
Case Description/Methods: Her total porphyrins were 20.1mcg/L, and random urine porphyrins were extremely elevated. Her Porphobilinogen Deaminase (PBGD) level was diminished, and was found to have a PBGD mutation. She was diagnosed with Acute Intermittent Porphyria. She was treated with hemin infusions with mild improvement in her symptoms, and oral glucose loading at onset of symptoms. However, her symptoms eventually came back, and she was initiated on Givosiran.
Discussion: Acute intermittent porphyria is an autosomal dominant condition with low penetrance of a mutation in the porphobilinogen deaminase (PBGD) gene, which leads to an accumulation of heme intermediates. Around 90% of carriers are asymptomatic, and thus, the prevalence is difficult to ascertain.
Abdominal pain is often the initial presenting symptom, and is characteristically severe & unremitting. It can be associated with other GI symptoms, including nausea, vomiting & diarrhea.
Neurologic symptoms, including peripheral neuropathy and muscle weakness can occur. Psychologic symptoms can also be present, including irritability, anxiety, paranoia & altered consciousness.
During an acute AIP attack, hyponatremia may also occur, and may lead to seizures.
The primary management of the disease revolves around prevention of attacks, including avoiding implicating medications, hormonal contraception, low-carb diets & alcohol. Pharmacologic therapy, including Givosiran, can also be used.
Disclosures:
Alexandra Scanameo indicated no relevant financial relationships.
Shefali Amin indicated no relevant financial relationships.
Andrew Lee indicated no relevant financial relationships.
John Altomare indicated no relevant financial relationships.
Alexandra Scanameo, MS, MS1, Shefali Amin, DO, MSEd2, Andrew E. Lee, MD3, John F. Altomare, MD4. B0613 - Acute Intermittent Porphyria, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
