Back

Poster Session A - Sunday Afternoon
Category: IBD
A0350 - Acute Severe Ulcerative Colitis Is Associated With an Increased Risk of Acute Pouchitis
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Hannah Posner, BS
Icahn School of Medicine at Mount Sinai
New York, NY
Presenting Author(s)
Hannah Posner, BS1, Maia Kayal, MD, MS1, Hadar Meringer Milwidsky, MD1, Michael Plietz, MD2, Sergey Khaitov, MD1, Patricia Sylla, MD1, Alexander J. Greenstein, MD, MPH3, Marla C. Dubinsky, MD4, Saurabh Mehandru, MD1, Jean-Frederic Colombel, MD1
1Icahn School of Medicine at Mount Sinai, New York, NY; 2Icahn School of Medicine at Mount Sinai, Waltham, MA; 3Mount Sinai Hospital, New York, NY; 4Susan and Leonard Feinstein IBD Center, Icahn School of Medicine, Mount Sinai, New York, NY
Introduction: Pouchitis occurs in up to 80% of patients with ulcerative colitis (UC) after total proctocolectomy (TPC) with ileal pouch anal anastomosis (IPAA). The pathogenesis of pouchitis is thought to involve a complex interaction between the microbiome and mucosal immune system, and increasing data suggest a robust immune system may be associated with an increased risk of pouchitis. We aimed to test this hypothesis by performing a retrospective cohort analyses comparing the incidence of acute pouchitis in patients admitted with acute severe ulcerative colitis (ASUC) at the time of colectomy to patients admitted without ASUC.
Methods: This was a retrospective cohort analysis of all patients with UC or IBD unclassified complicated by medically refractory disease or dysplasia who underwent TPC with IPAA at Mount Sinai Hospital between 2008 and 2017 and at least one subsequent pouchoscopy. ASUC was defined by the Truelove and Witts criteria. Acute pouchitis was defined according to the Pouchitis Disease Activity Index. Univariable cox regression was used to assess unadjusted relationships between hypothesized risk factors and acute pouchitis. Multivariable cox regression for the primary outcome of acute pouchitis was performed a priori with selection of the following clinically relevant variables: age, sex, ASUC admission, number of pre-colectomy biologics, and disease extent.
Results: A total of 416 patients met inclusion criteria. The median age at colectomy was 35.4 [IQR 26.1-49.0] years and 224 (53.8%) patients were male. Biologics were used in 292 (70.2%) patients pre-colectomy, and disease extent was reported as extensive in 327 (78.6%). Elective colectomy was performed in 251 (60.3%) patients. Of the 165 (39.7%) patients who underwent urgent colectomy, 77 (46.7%) were admitted with ASUC.
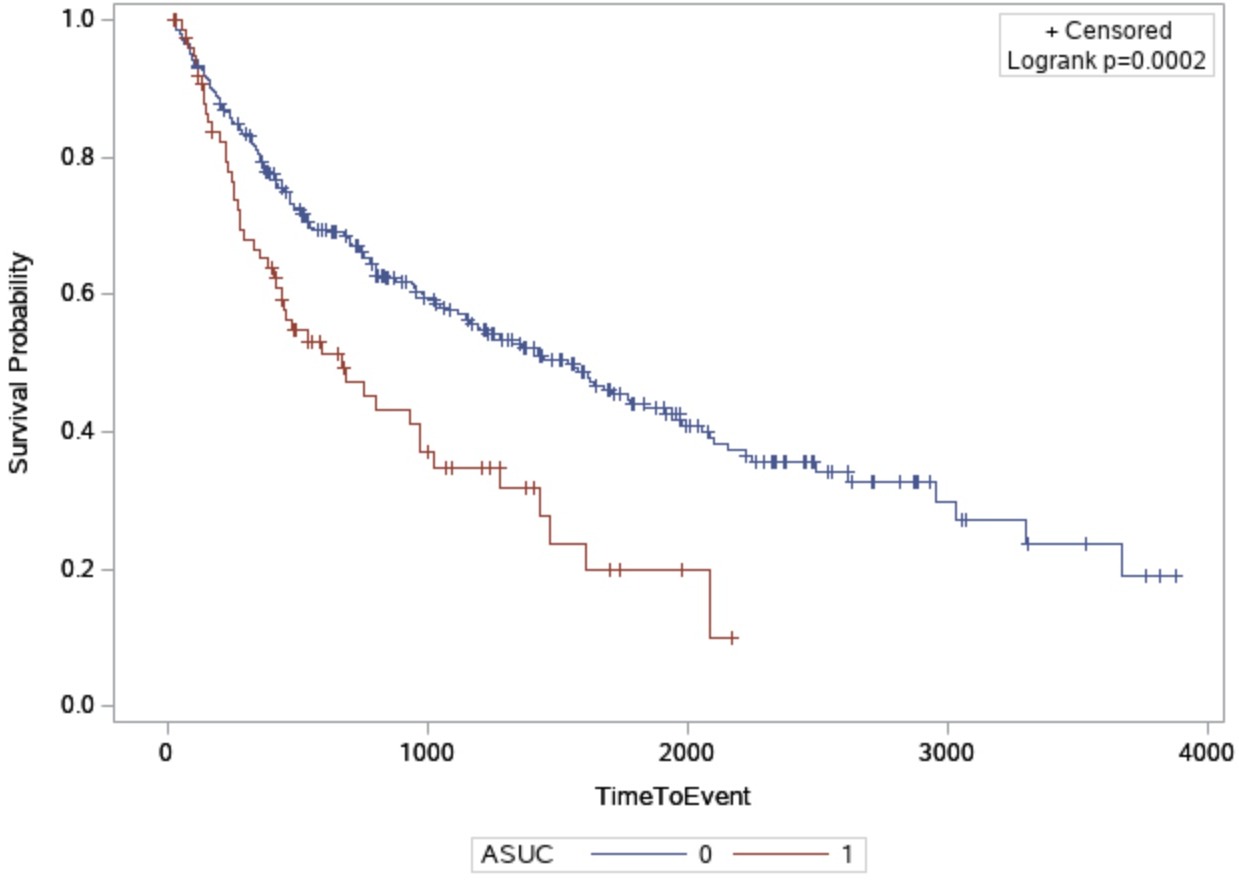
Acute pouchitis occurred in 228 (54.8%) patients a median of 1.3 [IQR 0.6-3.1] years after the final surgical stage. On multivariable analysis, older age at colectomy (HR 0.98 95% CI (0.97-0.99)) was significantly associated with a decreased probability of acute pouchitis, while ASUC (HR 1.53 95% CI (1.06-2.22)) and a greater number of biologics pre-colectomy (HR 1.30 95% CI (1.05-1.62)) were associated with an increased probability of acute pouchitis. Time to pouchitis was significantly less in patients admitted with ASUC compared to those not, p=0.002.
Discussion: ASUC at the time of colectomy was associated with an increased probability of acute pouchitis.
Disclosures:
Hannah Posner, BS1, Maia Kayal, MD, MS1, Hadar Meringer Milwidsky, MD1, Michael Plietz, MD2, Sergey Khaitov, MD1, Patricia Sylla, MD1, Alexander J. Greenstein, MD, MPH3, Marla C. Dubinsky, MD4, Saurabh Mehandru, MD1, Jean-Frederic Colombel, MD1. A0350 - Acute Severe Ulcerative Colitis Is Associated With an Increased Risk of Acute Pouchitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Icahn School of Medicine at Mount Sinai, New York, NY; 2Icahn School of Medicine at Mount Sinai, Waltham, MA; 3Mount Sinai Hospital, New York, NY; 4Susan and Leonard Feinstein IBD Center, Icahn School of Medicine, Mount Sinai, New York, NY
Introduction: Pouchitis occurs in up to 80% of patients with ulcerative colitis (UC) after total proctocolectomy (TPC) with ileal pouch anal anastomosis (IPAA). The pathogenesis of pouchitis is thought to involve a complex interaction between the microbiome and mucosal immune system, and increasing data suggest a robust immune system may be associated with an increased risk of pouchitis. We aimed to test this hypothesis by performing a retrospective cohort analyses comparing the incidence of acute pouchitis in patients admitted with acute severe ulcerative colitis (ASUC) at the time of colectomy to patients admitted without ASUC.
Methods: This was a retrospective cohort analysis of all patients with UC or IBD unclassified complicated by medically refractory disease or dysplasia who underwent TPC with IPAA at Mount Sinai Hospital between 2008 and 2017 and at least one subsequent pouchoscopy. ASUC was defined by the Truelove and Witts criteria. Acute pouchitis was defined according to the Pouchitis Disease Activity Index. Univariable cox regression was used to assess unadjusted relationships between hypothesized risk factors and acute pouchitis. Multivariable cox regression for the primary outcome of acute pouchitis was performed a priori with selection of the following clinically relevant variables: age, sex, ASUC admission, number of pre-colectomy biologics, and disease extent.
Results: A total of 416 patients met inclusion criteria. The median age at colectomy was 35.4 [IQR 26.1-49.0] years and 224 (53.8%) patients were male. Biologics were used in 292 (70.2%) patients pre-colectomy, and disease extent was reported as extensive in 327 (78.6%). Elective colectomy was performed in 251 (60.3%) patients. Of the 165 (39.7%) patients who underwent urgent colectomy, 77 (46.7%) were admitted with ASUC.
Acute pouchitis occurred in 228 (54.8%) patients a median of 1.3 [IQR 0.6-3.1] years after the final surgical stage. On multivariable analysis, older age at colectomy (HR 0.98 95% CI (0.97-0.99)) was significantly associated with a decreased probability of acute pouchitis, while ASUC (HR 1.53 95% CI (1.06-2.22)) and a greater number of biologics pre-colectomy (HR 1.30 95% CI (1.05-1.62)) were associated with an increased probability of acute pouchitis. Time to pouchitis was significantly less in patients admitted with ASUC compared to those not, p=0.002.
Discussion: ASUC at the time of colectomy was associated with an increased probability of acute pouchitis.
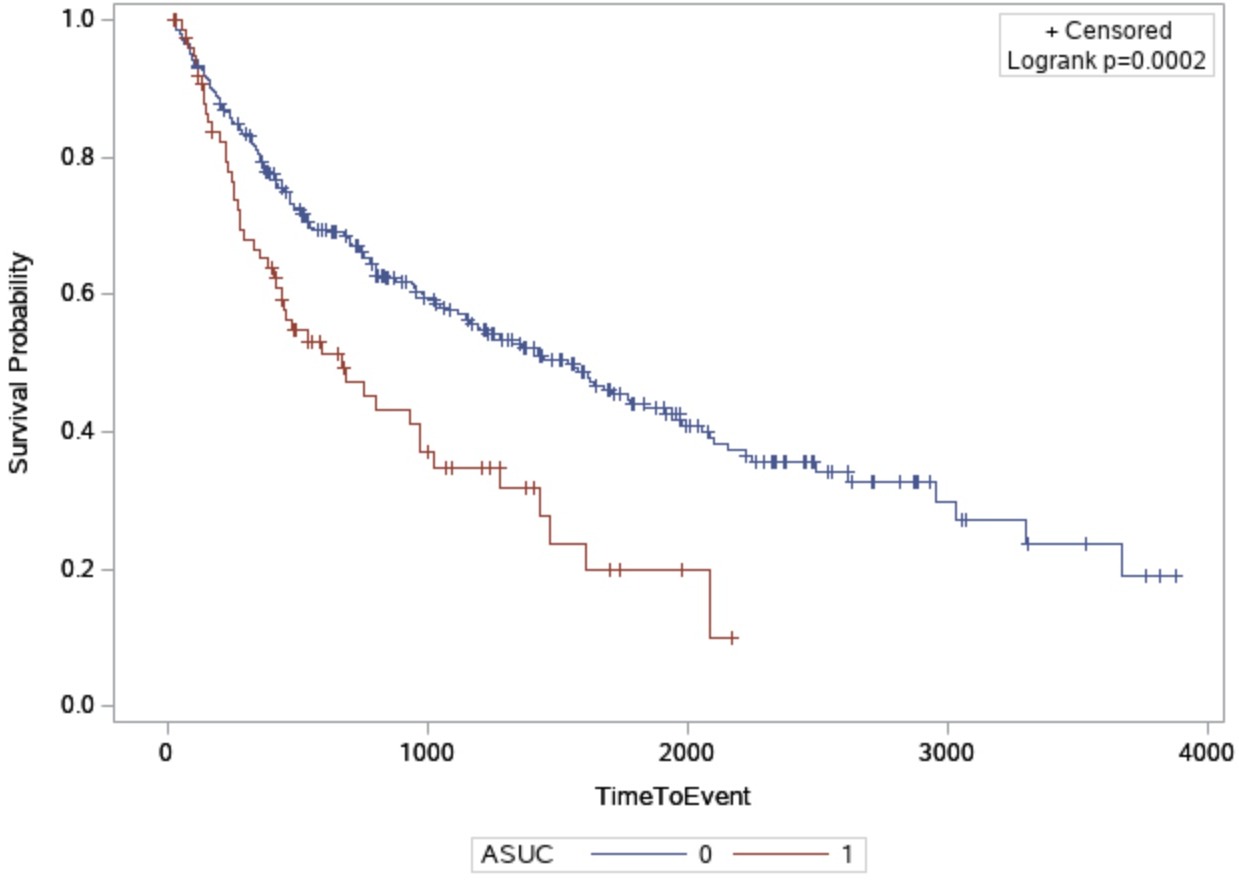
Figure: Kaplan-Meier estimates of developing acute pouchitis in patients with vs. without acute severe ulcerative colitis
Disclosures:
Hannah Posner indicated no relevant financial relationships.
Maia Kayal indicated no relevant financial relationships.
Hadar Meringer Milwidsky indicated no relevant financial relationships.
Michael Plietz indicated no relevant financial relationships.
Sergey Khaitov indicated no relevant financial relationships.
Patricia Sylla: Boston Scientific – Consultant. ColubrisMX – Consultant. Ethicon – Consultant. GI Windows – Consultant. Medtronic – Consultant. Neptune Medical – Consultant. Olympus – Consultant. Safeheal – Consultant. Stryker – Consultant.
Alexander Greenstein indicated no relevant financial relationships.
Marla Dubinsky: AbbVie – Consultant. Arena Pharmaceuticals – Consultant. Bristol Myers Squibb – Consultant. Celgene – Consultant. Eli Lilly – Consultant. Galapagos – Consultant. Genetech – Consultant. Gilead Sciences – Consultant. Janssen Pharmaceuticals – Consultant. Pfizer Inc – Consultant. Prometheus Laboratories – Consultant. Takeda – Consultant. Trellus Health – Shareholder. UCB – Consultant.
Saurabh Mehandru: Morphic – Consultant. Takeda – Advisory Committee/Board Member, Consultant.
Jean-Frederic Colombel: AbbVie – Consultant, Grant/Research Support. Amgen – Consultant. Arena – Consultant. BMS – Consultant. Boehringer Ingelheim – Consultant. Celgene Corporation – Consultant. Celltrion – Personal Fees. Eli Lilly – Consultant. Enterome – Personal Fees. Ferring Pharmaceuticals – Consultant. Galmed Research – Consultant. Galxo Smith Kline – Consultant. Genentech – Consultant. Genfit – Stock Options. Imedex – Consultant. Immunic – Consultant. Intestinal Biotech Development – Stock Options. Intestinal Biotech Development – Stock Options. Iterative Scopes – Consultant. Janssen Pharmaceuticals – Advisory Committee/Board Member, Consultant, Grant/Research Support. Kaleido Biosciences – Consultant. MedImmune – Personal Fees. Merck – Consultant. Microba – Consultant. Novartis – Consultant. PBM Capital – Consultant. Pfizer – Consultant. PPM Services – Personal Fees. Protagonist Therapeutics – Consultant. Sanofi – Consultant. Second Genome – Personal Fees. Seres – Personal Fees. Shire – Personal Fees. Takeda – Advisory Committee/Board Member, Consultant, Grant/Research Support. Theradiag – Personal Fees. TiGenix – Consultant. Vifor – Consultant.
Hannah Posner, BS1, Maia Kayal, MD, MS1, Hadar Meringer Milwidsky, MD1, Michael Plietz, MD2, Sergey Khaitov, MD1, Patricia Sylla, MD1, Alexander J. Greenstein, MD, MPH3, Marla C. Dubinsky, MD4, Saurabh Mehandru, MD1, Jean-Frederic Colombel, MD1. A0350 - Acute Severe Ulcerative Colitis Is Associated With an Increased Risk of Acute Pouchitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
